As more patients survive cancer, nursing education must meet the demand for nurses who can care for them.
Takeaways
- At the same time that death rates from cancer continue to decline, the numbers of cancer survivors are growing exponentially. For many of these survivors, cancer has become a chronic illness.
- Due to the increasing numbers of cancer survivors, nurses in most clinical settings, even those working outside of dedicated oncology units, are likely to care for survivors.
- Oncology nursing core competencies for all graduates of pre-licensure nursing programs have been developed to meet the care needs of cancer survivors.
The death rate from cancer in the United States peaked in 1991 and has decreased by almost 30% since then, leading to unprecedented numbers of cancer survivors. For many patients, cancer has become a chronic illness that requires long-term management of treatment sequelae and follow-up for recurrent disease. However, little attention has been given to the competencies required of non-oncology nurses caring for cancer survivors.
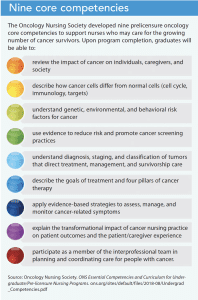
To address this need, a team of Oncology Nursing Society (ONS) staff and academic faculty developed nine core competencies for graduates of prelicensure nursing programs. These competencies, along with curriculum integration resources, provide an evidence-based framework to support nurse educators and nursing professional development specialists as they prepare a workforce skilled at caring for cancer survivors.
 Value of competencies
Value of competencies
Competence is fundamental to nursing practice. It’s demonstrated in the actual performance of a skill in a defined context and consistent with institutional policies. Competent performance involves the application of critical thinking, knowledge, technical, and interpersonal skills. Competence also implies a nurse has both the ability and capability to perform a job and achieve desirable outcomes. Competence has both a behavioral element, demonstrated as performance, and cognitive and affective components. The profile of a competent nurse is one who integrates knowledge and experience into practice, is proficient in skill performance, and has a caring, professional demeanor.
Core competency standards are developed by professional nursing organizations and are a tool for guiding nurses in the development of professional performance and functions. Specialty professional organizations like ONS develop specialty practice competencies to complement generalist core competencies and to define performance expectations when caring for unique, specialty patient populations.
Oncology competencies
Nurses new to practice can be challenged when caring for patients at risk for or living after a cancer diagnosis. To help ensure newly graduated nurses are competent in the care of patients with cancer, ONS developed prelicensure competencies. The competencies are designed to assist nurse educators in incorporating cancer care content into nursing school curricula such that the advanced beginner new graduate will have the knowledge, skills, and attitudes required for the provision of safe, high-quality care to patients with cancer.
The ONS competencies cover a range of content, including cancer pathophysiology, risk factors, genetic and environmental influences, risk reduction and screening, diagnosis, medical and surgical treatments, symptom management, impact on families and society, and interprofessional practice. (See Nine core competencies.) Collectively, the competencies provide the knowledge nurses need to assess, monitor, and evaluate the health status of patients with cancer in active treatment as well as cancer survivors and to provide safe, quality care. The competencies also serve as a benchmark to help nurses identify their personal knowledge gaps and skill limitations and to plan professional development. (See Putting core competencies into practice.)
Clinical nurses can put the nine oncology core competencies into practice by following these basic principles:
- Stay up-to-date on the most current recommendations for early detection and cancer screening practices.
- Recognize that symptom management is central to providing optimum care. Cancer and its treatments cause physical, emotional, and social effects that vary in presentation, intensity, and ability to mitigate.
- Use central vascular access devices to reduce repeated peripheral access. These devices are safe when managed according to guidelines for preventing infection and other complications.
- Provide palliative care as required to alleviate symptoms, and provide end-of-life care to promote death with dignity when cancer is advanced.
Keys to cancer survivor care
- Ask survivors about any symptoms they may be experiencing, including the frequency, duration, intensity, and level of associated distress.
- Know a patient’s cancer history. Assess for changes in health since receiving treatment.
- Ask patients if they have a cancer survivor care plan.
- If you’re working in an emergent care setting, be familiar with the presentation and management of oncology emergencies.
Manage professional development
- Identify gaps in knowledge and seek additional information.
- Attend conferences and take advantage of online learning options.
- Suggest oncology care as a topic to your organization’s/unit’s professional development specialist.
Creating curriculum resources
As part of ONS’s 2016-2019 strategic planning, the board of directors addressed the findings of two validation studies. (See Finding validation.) To accomplish the strategic goal of advancing the quality of cancer care and patient safety, the board developed this objective: Ensure the integration of oncology content into nursing curriculum. The board then formed a cross-functional workgroup consisting of marketing, communication, and learning and development staff. The workgroup developed a 2-hour interactive online course based on the new competencies that fits easily into existing prelicensure curriculum or serves as a strong oncology foundation for programs without such content.
One challenge to creating the essential curriculum was identifying the most important elements of caring for cancer survivors. As oncology care and basic scientific knowledge related to cancer experiences unprecedented disruptive innovations—moving from treatment based on tumor location (for example, the lungs) to treatments based on tumor cell genomics and mutations and personalized treatment plans—patients are living longer and experiencing toxicities and side effects new to the care team. For that reason, the workgroup focused the curriculum on supportive care (health promotion, risk identification, and strategies for living with cancer as a chronic condition and for living without evidence of cancer after treatment) of patients and their caregivers.
Two national studies, funded by the Susan G. Komen Foundation for the Cure and sponsored by the Oncology Nursing Society (ONS), provided the groundwork for ONS to develop oncology core competencies for prelicensure nursing programs. One study looked at the faculty perspective and the other at medical-surgical and oncology RN perspectives.
Faculty perspective
The first study captured the faculty perspective on the depth and importance of cancer content taught to nursing students during their prelicensure preparation in 931 accredited nursing schools (53 diploma, 347 associate, and 531 baccalaureate). Results revealed that the importance of these concepts was rated consistently higher than the depth at which it was currently taught. Lack of time in packed nursing curricula was cited as the top challenge faculty faced in teaching oncology content; other challenges included limited access to cancer care experts, clinical sites, and resources.
Medical-surgical and oncology RN perspectives
The second study set out to determine the learning needs of new graduate nurses in non-oncology settings who care for cancer survivors after their acute treatment. Medical-surgical (n = 313) and oncology nurses (n = 302) were asked to rate the depth and importance of content non-oncology nurses need to care for cancer survivors. Findings were similar to the faculty perspective study, with the importance of cancer content rated higher than the depth at which it was currently taught. Both groups of nurses identified symptom management concepts among the top learning needs. Barriers cited in caring for oncology patients admitted to non-oncology clinical settings included lack of time to learn about patient needs, limited knowledge, and no access to cancer resources.
Sources: Lockhart et al. 2013 and Lockhart et al. 2018
To achieve their education and dissemination objectives, the workgroup completed an environmental scan that included reviewing the American Association of Colleges of Nursing (AACN) Essentials of Baccalaureate Education for Professional Nursing Practice, the National Council of State Boards of Nursing Strategic Practice Analysis, and the current literature regarding innovative curriculum strategies for cancer care education. After the scan, representatives from ONS met with nursing education experts at AACN and the National League for Nursing for further discussions related to cancer care education. Findings from the environmental scan and discussions informed the workgroup’s concise, two-pronged educational strategy—one prong student focused and the other faculty focused.
Student content
The student-focused content is a 2-hour online course housed within the ONS learning management system. Before accessing the course, students complete a baseline assessment of their oncology knowledge. The curriculum is presented in a series of eight chapters that emphasize survivorship and the core competencies. (See Chapter by chapter.) The baseline assessment questions are integrated into the course so learners can gauge improvements in their knowledge. Students receive a certificate of completion at the end of the course.
Faculty content
Oncology clinical nurse specialists (members of the workgroup) and nurse educators with oncology expertise developed the faculty-focused content (including PowerPoint presentations to support classroom lectures) using ONS educational resource center materials. Faculty members can upload the presentations to a learning management system for student review before class or clinical activities. Other faculty-focused materials include case studies, fast-fact sheets, learning activities, and test questions.
The Oncology Nursing Society essential oncology content includes a 2-hour online course broken down into eight chapters.
1 What is cancer?
2 What causes cancer?
3 Cancer risks and prevention
4 Cancer diagnosis and staging
5 What are treatments for cancer?
6 The nurse’s role: Symptom management
7 The nurse’s role: Survivorship care and care coordination
8 The nurse’s role: Ethics and patient advocacy
To help nurse educators without oncology expertise build their confidence and skills to teach content related to the nine core competencies, the workgroup developed a faculty manual to correspond with the eight-chapter online student course. The manual provides narratives to support the presentations and offers suggestions for using case studies and accompanying materials for classroom and clinical activities. For example, a lecturer might present content related to the nurse’s role in survivorship care and care coordination during class, and a clinical instructor might then use slides and fast-fact sheets to help students develop survivorship care plans (including a record of care received, important disease characteristics, and a follow-up care plan incorporating evidence-based standards related to maintaining health and living well after cancer treatment). (For more information about the curriculum resources, contact research@ons.org.)
Redefining care
As the number of cancer survivors increases (by 2026, the number of survivors in the United States is expected to exceed 20 million), the demand for providers and nurses with oncology expertise will outpace supply. To redefine care expectations in this survivorship era, ONS developed nursing core competencies that are being implemented in U.S. prelicensure programs. The new competencies and companion curriculum-integration materials, created by experienced oncology nurse educators, provide a foundation for preparing a nursing workforce ready to care for cancer survivors and ensure optimal quality, safety, and clinical outcomes.
Melinda G. Oberleitner is the dean of the college of nursing and allied health professions, a professor in the department of nursing, and SLEMCO/BORSF Endowed Professor in Nursing at University of Louisiana at Lafayette. Joan Such Lockhart is a professor and MSN nursing education track director at Duquesne University School of Nursing in Pittsburgh, Pennsylvania. Janet S. Fulton is a professor and associate dean for graduate programs at Indiana University
School of Nursing in Indianapolis. Deborah Struth is a research associate at the Oncology Nursing Society in Pittsburgh, Pennsylvania.
References
American Association of Colleges of Nursing. The Essentials of Baccalaureate Education for Professional Nursing Practice. 2008. aacnnursing.org/Portals/42/Publications/BaccEssentials08.pdf
American Cancer Society. Cancer Facts and Figures 2019. cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf
Cowan DT, Norman I, Coopamah VP. Competence in nursing practice: A controversial concept—A focused review of literature. Nurse Educ Today. 2005;25(5):355-62.
Lockhart JS, Galioto M, Oberleitner MG, et al. A national survey of oncology content in prelicensure registered nurse programs. J Nurs Educ. 2013;52(7):383-90.
Lockhart JS, Oberleitner MG, Felice TL, Vioral A. Using evidence to prepare non-oncology nurses for cancer survivor care. J Contin Educ Nurs. 2018;49(1):12-18.
Lubejko BG, Wilson BJ. Oncology Nursing: Scope & Standards of Practice. Pittsburgh, PA: Oncology Nursing Society; 2019.
Pirschel C, Lockhart JS, Oberleitner M. What the research says about supporting cancer survivors in non-oncology settings. ONS Voice. September 6, 2018. voice.ons.org/news-and-views/what-the-research-says-about-supporting-cancer-survivors-in-non-oncology-settings
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA: Cancer J Clin. 2019;69(1):7-34.


















