Recognize symptoms, report promptly
- More than 600 anticholinergic medications exist.
- Nurses play an important role in reducing anticholinergic burden in patients with multiple conditions.
- Recognizing the significant side effects associated with multiple anticholinergic medications can help nurses identify and intervene promptly.
Anticholinergics, widely used in clinical practice for an extensive range of diseases, exert effects on circulation, respiration, alertness, and vision by blocking the action of acetylcholine (a neurotransmitter) within the cholinergic system. Acetylcholine plays an important role in normal brain and body function by producing and communicating signals between neurons in the central system (CNS) and peripheral nervous system (PNS). Most of the body’s movements (including muscle activation, smooth muscle contraction, blood vessel dilation, body secretion, and heart rate reduction) are directly related to acetylcholine.
Within the CNS, acetylcholine affects motivation, arousal, attention, learning, and memory, as well as rapid eye movement during sleep. It’s produced in cholinergic neural cells by synthesizing choline and acetyl-coenzyme A in the terminal end of the nerve’s cytoplasm. Primary sources of choline come from food, such as meat, fish, dairy, eggs, whole grains, legumes, nuts, broccoli, cabbage, apples, and tangerines. The National Institutes of Health recommends a daily choline intake of 550 mg for men and 425 mg for women. Estrogen helps to stimulate choline.
The cholinergic system uses muscarinic (present on target organ cells within the parasympathetic nervous system) and nicotinic (primarily found on the nerves in the autonomic nervous system) receptors. Anticholinergic medications predominately affect muscarinic receptors.
Anticholinergic effects
Currently, more than 600 specific medications exhibit anticholinergic effects—many of which cause adverse rather than therapeutic effects. Anticholinergics decrease or block the actions of acetylcholine on the PNS receptors on smooth muscle cells, glands, and the CNS. They also act as muscarinic antagonists to block muscarinic cholinergic receptors, potentially leading to mydriasis (dilated pupils), bronchodilation, increased heart rate, and inhibition of secretions. (See Drugs to watch for.)
Drugs to watch for
The following drug classes have anticholinergic properties:
Neuropsychiatric medications
Antidepressants
Antiepileptics
Antiparkinsonians
Antipsychotics
Benzodiazepines
Opioids
Tricyclic antidepressants
Z-sleep medications
Nonpsychoactive medications
Antihistamines
Antispasmodics
Bronchodilators
Cardiovascular medications
Diuretics
Corticosteroids
GI medications
Muscle relaxants
Neuropathic pain medications
Urologic medications
Source: López-Álvarez et al, 2019
Because many of the most frequently prescribed medications have anticholinergic properties, researchers have investigated anticholinergic burden (ACB) through available scales. The literature describes several scales primarily focused on patients 65 years and older; no consensus exists on which scale is most sensitive or widely accepted.
Anticholinergic burden
To investigate the risks of ACB, Hanlon and colleagues performed a longitudinal analysis of 502,538 subjects age 37 to 73 years. Using 10 scales, they found that ACB was associated with anticholinergic prescribing in mid- to older-aged populations at a rate of 8% to 17.6%, depending on the scale used. Increased ACB was directly associated with mortality, cardiovascular events, falls, fractures, cognitive changes, dementia, and delirium. (See Adverse effects.)
Adverse effects
Anticholinergic medications have the following adverse effects on the central and peripheral nervous systems.
Central nervous system effects
Acceleration of neurodegenerative processes
Brain atrophy (long-term use)
Confusion
Cognitive dysfunction and impairment
Functional disturbances (such as falls)
Psychotic symptoms
Sedation
Peripheral nervous system effects
Blurred vision/dilated pupils
Constipation
Dry eyes
Dry mouth
Flushed skin (inability to sweat)
Increased heart rate
Paralytic ileus
Urinary retention
Source: López-Álvarez et al, 2019
Additional studies analyzed by Hanlon and colleagues have found a 12.5% prevalence of prescribed anticholinergics for older adults in the primary care setting. In elderly patients with memory changes, prevalence increased to 25.8%. Hospitalized elderly patients had 79% of prescribed anticholinergic use, and of patients with mild cognitive changes seen in a memory clinic, 44.7% were taking multiple anticholinergic medications.
Older adult risk
A 20-year longitudinal study by Wouters and colleagues investigated the effects of long-term use of anticholinergics and sedative medications on cognitive and physical function in later life. They confirmed an association between long-term cumulative exposure to anticholinergics and sedatives and worsened cognitive and physical functioning. A systematic review and meta-analysis by Dmochowski and colleagues evaluated the use of anticholinergics for more than 3 months on dementia and cognitive function. They found an average 46% increased risk of dementia compared to nonuse.
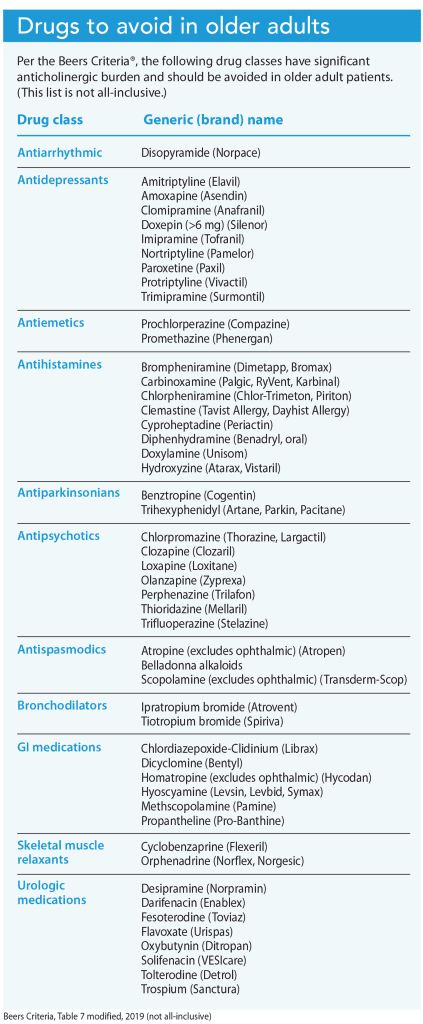
The American Geriatric Society’s Beers Criteria® identify potentially inappropriate medication use in older adults. The 2019 update identifies a table of drugs with strong anticholinergic properties that should be avoided in older patients. (See Drugs to avoid in older adults.)
Nursing implications
Nurses must be able to recognize and report symptoms that may indicate ACB or toxicity. You also must know about and understand the physiologic effects associated with anticholinergics. Consider the muscarinic receptors in the brain, eye, salivary and sweat glands, heart, lungs, GI tract, bladder, and skin when evaluating patients.
Use the following historical mnemonic to help identify significant symptoms associated with anticholinergic medications:
- Hot as a hare (fever)
- Red as a beet (skin vasodilation)
- Blind as a bat (pupil dilation)
- Dry as a bone (dry mouth, skin, reduced sweating)
- Mad as a hatter (delirium, confusion, hallucinations)
- Full as a flask (urinary retention)
- Stuffed as a pepper (constipation)
When you’re familiar with the effects associated with anticholinergics you can prevent an escalation of symptom severity by promptly reporting your suspicions to the prescriber, who can discontinue the medication. Ensuring adequate hydration, applying skin moisturizers, minimizing bright lights, adjusting the environmental temperature, and evaluating bowel and bladder function are simple but effective interventions to reduce anticholinergic effects. Given the growing number of older adult patients, all nurses must be able to recognize these symptoms.
Kim Kuebler is the director and founder of Multiple Chronic Conditions Resource Center in Pleasant Lake, Michigan.
American Nurse Journal. 2023; 18(8). Doi: 10.51256/ANJ082348
References
American Geriatrics Society. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674-94. doi:10.1111/jgs.15767
Cafasso J. Anticholinergics. Healthline. February 14, 2023. healthline.com/health/anticholinergics
Cherry K. How acetylcholine functions in your body. Verywell Mind. May 30, 2023. verywellmind.com/what-is-acetylcholine-2794810
Dmochowski RR, Thai S, Iglay K, et al, Increased risk of incident dementia following use of anticholinergic agents: A systematic literature review and meta-analysis. Neurourol Urodyn.2021;40(1):28-37. doi:10.1002/nau.24536
Food and Drug Administration. Taking Z-drugs for insomnia? Know the risks. April 30, 2019. fda.gov/consumers/consumer-updates/taking-z-drugs-insomnia-know-risks
Ghossein N, Kang M, Lakhkar AD. Anticholinergic medications. StatPearls. May 8, 2023. ncbi.nlm.nih.gov/books/NBK555893
Gorup E, Rifel J, Petek Šter M. Anticholinergic burden and most common anticholinergic-acting medicines in older general practice patients. Zdr Varst. 2018;57(3):140-7. doi:10.2478/sjph-2018-0018
Hanlon P, Quinn TJ, Gallacher KI, et al. Assessing risks of polypharmacy involving medications with anticholinergic properties. Ann Fam Med. 2020;18(2):148-55. doi: 0.1370/afm.2501
Lattanzio F, Corica F, Schepisi R, et al. Anticholinergic burden and 1-year mortality among older patients discharged from acute care hospital. Geriatr Gerontol. 2018;18(5):705-13. doi:10.1111/ggi.13234
López-Álvarez J, Sevilla-Llewellyn-Jones J, Agüera-Ortiz L. Anticholinergic drugs in geriatric psychopharmacology. Front Neurosci. 2019;13:1309. doi:10.3389/fnins.2019.01309
The University of British Columbia. How well do you know your anticholinergic (antimuscarinic) drugs? ti.ubc.ca/2018/09/10/113-anticholinergic-antimuscarinic-drugs/
The Royal Children’s Hospital Melbourne. Anticholinergic syndrome. August 2017. rch.org.au/clinicalguide/guideline_index/Anticholinergic_Syndrome/
Wouters H, Hilmer SN, Gnjidic D, Van Campen JP, et al. Long-term exposure to anticholinergic and sedative medications and cognitive and physical function in later life. J Gerontol A Biol Sci Med Sci. 2020;75(2):357-65. doi:10.1093/gerona/glz019
Key words: anticholinergics, anticholinergic burden, polypharmacy, medication safety