An unexpected fall from a ladder, a motor vehicle accident, a sudden onset of acute chest pain…these are merely a few of the reasons people find their daily lives disrupted and seeking care in an emergency department (ED). Once in the ED, they are often among many others seeking care. The nurse must then use triage to prioritize patients.
Triage of incoming patients is a complex process that is frequently misunderstood by the layperson. The word triage comes from the French verb “trier” which means “to sort”. In essence, the triage nurse is constantly “sorting” by prioritizing and re-prioritizing the incoming ill or injured patients who require care. The nurse should base his or her decision-making on evidence, not only to ensure patients receive the care they need when they need it, but also because patients often misunderstand the triage process. Explaining that there is a process behind decisions may help ease anxiety.
In Fast Facts for the Triage Nurse: Orientation and Care Guide Second Edition, Deb Jeffries MSN-Ed, RN-BC, CEN, CPEN writes about triage acuity scales used in EDs around the world.
TRIAGE ACUITY: OVERVIEW
Emergency departments (EDs) have historically used triage scales or rating systems that were highly subjective, with little to no research as to their reliability and validity. Today, validated and reliable 5-level emergency department triage scales (Emergency Severity Index – ESI and the Canadian Triage and Acuity Scale – CTAS) are used almost exclusively in the United States as well as elsewhere across the globe. In addition to ESI and CTAS there are other 5-level triage scales used globally including but not limited to the Australasian Triage Scale (ATS) and the Manchester Triage System (MTS). Each of these scales will be briefly reviewed.
Nurses have often lacked formal education related not only to the use of triage acuity scales but also to the triage process as a whole. Unfortunately, just having a nursing license and being alive continues to be the only qualifications required by some facilities for a nurse to be assigned to the triage role. This is a dangerous practice and the reader is encouraged to review the Emergency Nurses Association Position Statement Triage Qualifications and Competency to gain insight into best practice regarding triage qualifications and competency. Regardless of the specific triage acuity scale used, nurses must receive comprehensive education regarding the use of that scale. Appropriate use of a valid and reliable 5-level triage acuity scale provides discrimination between acuity levels and allows the nurse to safely determine who can and cannot wait for care.
Fast Facts
• Nurses providing care at the stretcher-side can attest to the complexity of the patients seen in most EDs today. For the triage nurse, assigning the correct acuity level is first and foremost a patient safety issue.
• Assigning a correct acuity level can help staff obtain the resources needed to provide appropriate and effective patient care. However, this can only be a reality if we use a common language that communicates to strategic leaders how sick the patients really are.
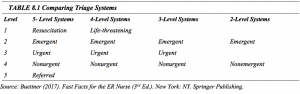
Depending on the triage acuity scale utilized, specific criteria help the triage nurse determine the level assigned to each patient. Table 8.1: Comparing Triage Systems provides insight into the categories that are used internationally with a 5 level triage system supported by both the Emergency Nurses Association (ENA) and the American College of Emergency Physicians (ACEP).
ENA and ACEP have a joint position statement regarding Triage Scale Standardization located at https://www.ena.org/docs/default-source/resource-library/practice-resources/position-statements/supported-statements/triage-scale-standardization.pdf?sfvrsn=a940caa_4
Be sure to base your triage decisions on established scales. Use your knowledge, experience, critical thinking, and intuition to ask the right questions and assess the right body systems to help determine the most appropriate level of urgency. Sometimes the subtle clues may not be visible to the eye, yet are the critical elements that help determine the most appropriate triage acuity level.
Reproduced with permission from Springer Publishing Company from Fast Facts for the Triage Nurse (2ndEd.). New York, NY: Springer Publishing.
Lynn Sayre Visser is the author of Fast Facts for the Triage Nurse (2ndEd.) and Rapid Access Guide for Triage and Emergency Nurses. She has devoted her career to emergency nursing, triage education, and mentoring others.
*This blog is the second in a series. Read the third blog here.


















