Tom Anderson, age 74, was admitted to the telemetry unit yesterday with new onset of chest pain. Melanie, his nurse, notes that his troponin test came back negative, and a stress test is planned for later today. A former smoker, Mr. Anderson has a history of hypertension and no known allergies. His home medications include lisinopril 20 mg and hydrochlorothiazide 12.5 mg. Daily aspirin was added to his regimen in the hospital yesterday.
A few hours into Melanie’s shift, Mr. Anderson pushes the call light. When Melanie enters his room, he tells her he is short of breath and feels like he has a lump in his throat.
History and assessment hints
On assessment, Melanie finds Mr. Anderson anxious and dyspneic, with swelling of the left side of his face and lips. She quickly obtains his vital signs: respiratory rate 38 breaths/minute, heart rate 140 beats/minute, blood pressure 100/60 mm Hg, and oxygen saturation (O2 sat) 90%. He seems to have trouble speaking as he tells Melanie his tongue feels swollen.
When Melanie assesses his lung sounds, she hears stridor but finds his lungs are clear. When she examines his tongue, she sees edema on the left side. Realizing he might be having an allergic reaction, she immediately calls the rapid response team (RRT).
On the scene
By the time the RRT team arrives, Mr. Anderson has become even more short of breath, and his blood pressure has dropped to 90/50 mm Hg. The team administers 100% oxygen by nonrebreather mask and starts infusing 0.9% normal saline solution.
The physician orders epinephrine 1:1000 at 0.3 mL intramuscularly (to reverse systemic hypotension, vascular permeability, and bronchospasm), along with methylprednisolone 125 mg I.V. and ranitidine 50 mg I.V. (to block the effects of histamine and other inflammatory mediators). Shortly after receiving epinephrine, Mr. Anderson begins to breathe more easily and his blood pressure rises to 112/60 mm Hg.
Outcome
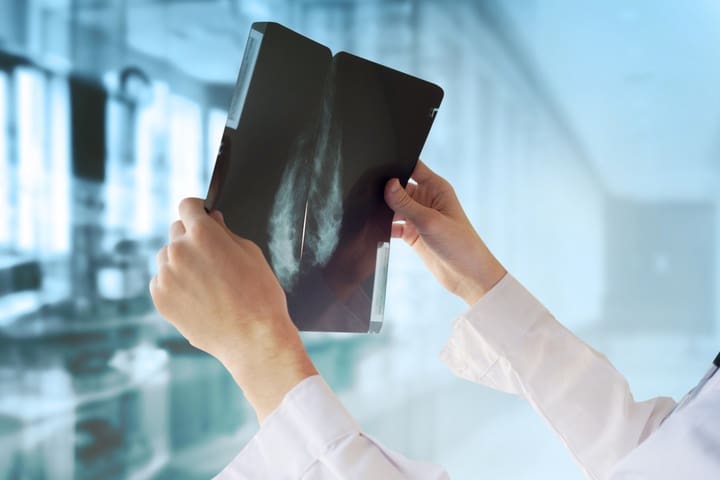
After reviewing Mr. Anderson’s medication list, clinicians suspect his difficulty speaking, swollen tongue, and stridor resulted from angioedema caused by lisinopril, an angiotensin-converting enzyme inhibitor (ACEI). ACEIs block activity that stimulates transformation of angiotensin I to angiotensin II, leading to an increase in bradykinin, which in turn lowers blood pressure and increases capillary permeability.
Once his blood pressure and breathing stabilize, Mr. Anderson is transferred to the intensive care unit for closer observation. He continues to receive ranitidine 50 mg I.V. every 8 hours and methylprednisolone (lowered to 60 mg) I.V. every 6 hours, along with diphenhydramine 25 mg I.V. every 6 hours. His vital signs remain stable, and no other signs or symptoms occur.
Education and follow-up
Marked by localized nonpruritic, nonpitting edema of the skin and subcutaneous tissues, angioedema stems from rapid plasma extravasation from the capillaries caused by high bradykinin levels. Angioedema related to ACEI therapy usually arises shortly after drug initiation, but it can occur at any time during drug therapy.
Signs and symptoms include transient swelling of the skin and mucous membranes, typically affecting the face, lips, tongue, oropharynx, and upper respiratory tract. Life-threatening upper-airway edema also may occur. Recognizing mild symptoms early is crucial, because rapid progression can lead to a severe and possibly irreversible outcome.
Angioedema is more common in African-Americans, Asians, females, people older than age 65, smokers, and persons with C1 esterase inhibitor deficiency or a history of asthma or urticaria. Adding another drug known to cause angioedema to an ACEI can increase angioedema risk.
The physician discontinues Mr. Anderson’s ACEI therapy and instructs him to avoid ACEIs for the rest of his life. On the patient’s discharge, Melanie documents his angioedema history in his permanent medical record and urges him to purchase a medical alert bracelet to identify his allergies.
References
Beltrami L, Zanichelli A, Zingale L, et al. Long-term follow-up of 111 patients with angiotension-converting enzyme inhibitor-related angioedema. J Hypertens. 2011;29(11):2273-7.
Calderia D, David C, Sampaio C. Tolerability of angiotension-receptor blockers in patients with intolerance to angiotension-coverting enzyme inhibitors. Am J Cardiovasc Drugs. 2012;12(4):263-77.
Campo P, Fernandez TD, Canto G, Mayorga C. Angioedema induced by angiotensin-converting enzyme inhibitors. Curr Opin Allergy Clin Immunol. 2013;13(4):337-44.
Flattery MP. When ACE inhibitors cause angioedema. Am Nurse Today. 2011;6(4).
Kuhlen JL, Forcucci J. Angiotensin-converting enzyme inhibitor-induced unilateral tongue angioedema. Am J Med Sci. 2012;344(5):416-7.
Nia AM, Er F. Angioedema associated with the use of angiotensin-converting enzyme inhibitors. CMAJ. 2013;185(1):E80.
Zuraw BL, Bernstein JA, Lang DM, et al.; American Academy of Allergy, Asthma and Immunology; American College of Allergy, Asthma and Immunology. A focused parameter update: hereditary angioedema, acquired C1 inhibitor deficiency, and angiotensin-converting enzyme inhibitor-associated angioedema. J Allergy Clin Immunol. 2013;131(6):1491-3.
Cindy Ruiz is a clinical nurse specialist in critical care at Northwest Community Hospital in Arlington Heights, Illinois.