Use an assessment tool to prompt discussion and increase patient engagement.
- An estimated 34 million Americans age 18 years and older have diabetes; type 2 diabetes is the most common and places patients at a higher risk for cardiovascular disease.
- Many ambulatory clinics that serve lower socioeconomic populations with limited health literacy miss opportunities to address the risk of severe illness and death related to unmanaged or undiagnosed atherosclerotic cardiovascular disease
- An embedded electronic health record or manual calculation tool, such as an ASCVD risk score, creates a visual reminder for providers to assess risk levels, provide education, and engage patients in actively participating in their care.
An estimated 34 million Americans, age 18 years and older, have diabetes, most with type 2 diabetes (T2DM) as well as a high risk for cardiovascular disease (CVD). More than 80% of patients with diabetes meet or rank above the Centers for Disease Control and Prevention risk levels for hemoglobin A1c (HbA1c), blood pressure, cholesterol, and smoking, leading to cardiac-related conditions such as atherosclerotic cardiovascular disease (ASCVD). Early counseling and intervention in ambulatory care settings, via risk assessment screening for early detection, can help reduce modifiable ASCVD risks. (See Risk assessment: History and recommendations.)
Risk assessment: History and recommendations
The American College of Cardiology (ACC) presented findings from a Swedish study, which noted that out of 19,105 deaths of patients with type 2 diabetes (T2DM), almost 60% were related to heart disease. The study also reported a 71% to 87% higher risk for populations of lower socioeconomic status. To improve outcomes, the ACC and American Heart Association (AHA) 2013 and 2019 guidelines for assessing cardiovascular risk and cholesterol management recommend using an atherosclerotic cardiovascular disease (ASCVD) 10-year risk estimation tool, either embedded within the electronic health record (EHR) or via an online calculator, for improved disease management in adults with T2DM between the ages of 40 and 79 (the most recent calculator is recommended for those between 20 and 79 years).
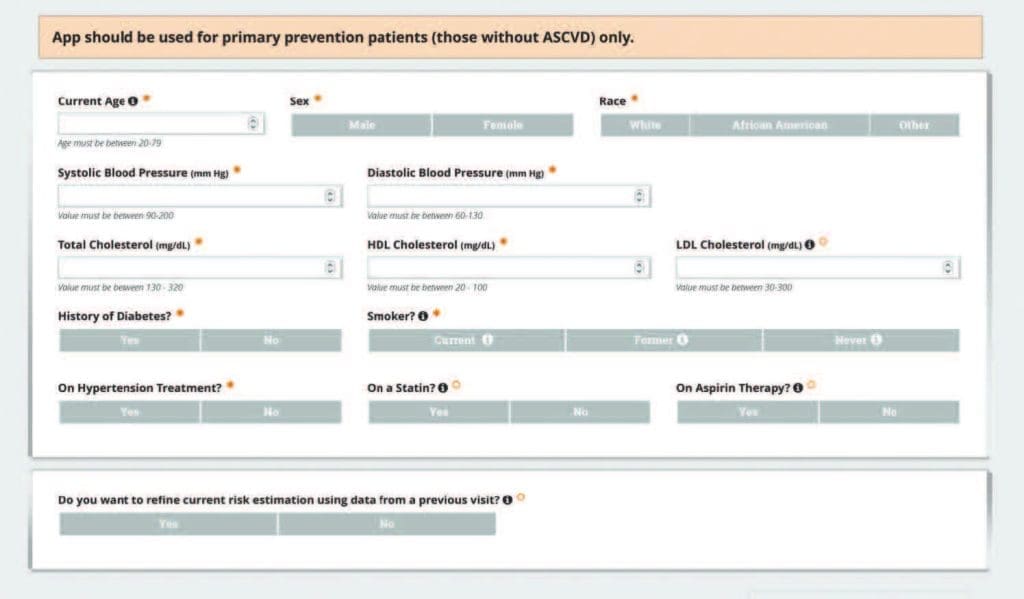
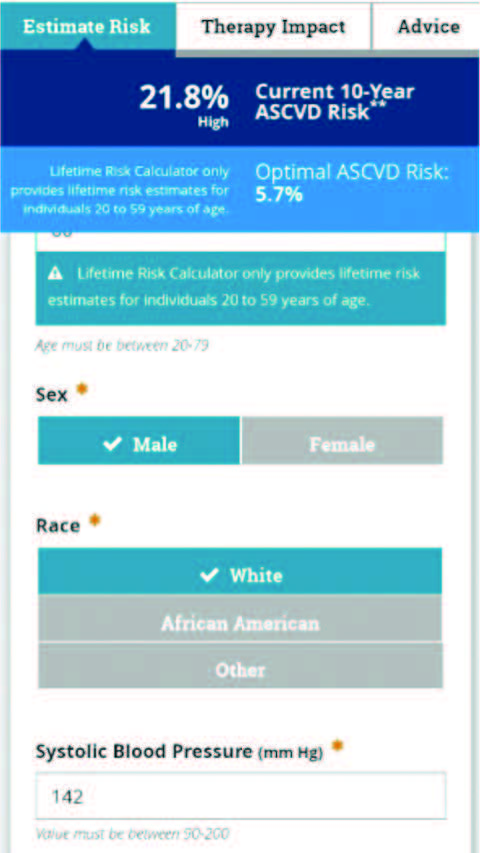
The ACC/AHA risk estimator tool can calculate a risk percentage for current and future cardiovascular disease using specific criteria of diabetes history, high-density lipoprotein, low-density lipoprotein, total cholesterol, smoking history, age, gender, race, systolic and diastolic blood pressure, current use of a statin, hypertension (HTN) medications, and aspirin. The tool also is recommended by the American Diabetes Association in partnership with the AHA for the Know Diabetes by Heart™ program, which guides nursing and provider collaboration for patient education, improved self-management, and early treatment recommendations.
Based on evidence that proves early counseling and interventions help reduce modifiable cardiovascular risks associated with HTN, heart attack, and stroke, the Agency for Healthcare Research and Quality, along with Healthy People 2020, also strongly suggest consistent ambulatory cardiovascular risk screenings in adults with T2DM. Missed ASCVD screenings can create lost opportunities for risk stratification, which may help decrease the risk of severe illness and death in disparate communities.
Many ambulatory clinics serve patients in lower socioeconomic communities who may have limited health literacy. An embedded electronic health record (EHR) tool, such as an ASCVD risk score, creates a visual reminder for providers to assess a patient’s risk level, provide education, and engage them in their care. (See Risk assessment tools.)
Risk assessment tools
Several cardiovascular risk assessment tools exist, and comparison studies have helped clarify their accuracy.
- In 2019, a cross-sectional study comparing the American College of Cardiology/American Heart Association (ACC/AHA) atherosclerotic cardiovascular disease (ASCVD) risk calculator tool and the United Kingdom Prospective Diabetes Study Risk engine tools aimed to understand which was most appropriate for adult patients with type 2 diabetes (T2DM). The results supported the ACC/AHA ASCVD risk calculator as the most reliable for current and future risk assessment.
- Another cross-sectional study by Hong and colleagues compared the ASCVD risk tool to the China-PAR Project (Prediction for ASCVD Risk in China) assessment, with an outcome recommending the use of the ASCVD risk score to guide providers in earlier treatment options.
- In 2021, a cohort study called the Learnings with Experts to Advance Diabetic Dyslipidemia Management in India presented analyses of 199 primary clinic sites. The study assessed whether the 2018 American Diabetes Association T2DM guidelines and the ASCVD risk calculator were consistently used for risk scoring and appropriate treatment approaches. Because of missed stratification opportunities from uncompleted ASCVD risk calculations, most patients with T2DM weren’t appropriately prescribed statin medications.
As a tool for clinic or mobile use, the ACC Foundation Risk Estimator Plus app can be downloaded to the computer (left) or as a tablet or smartphone Android or Apple app (right).
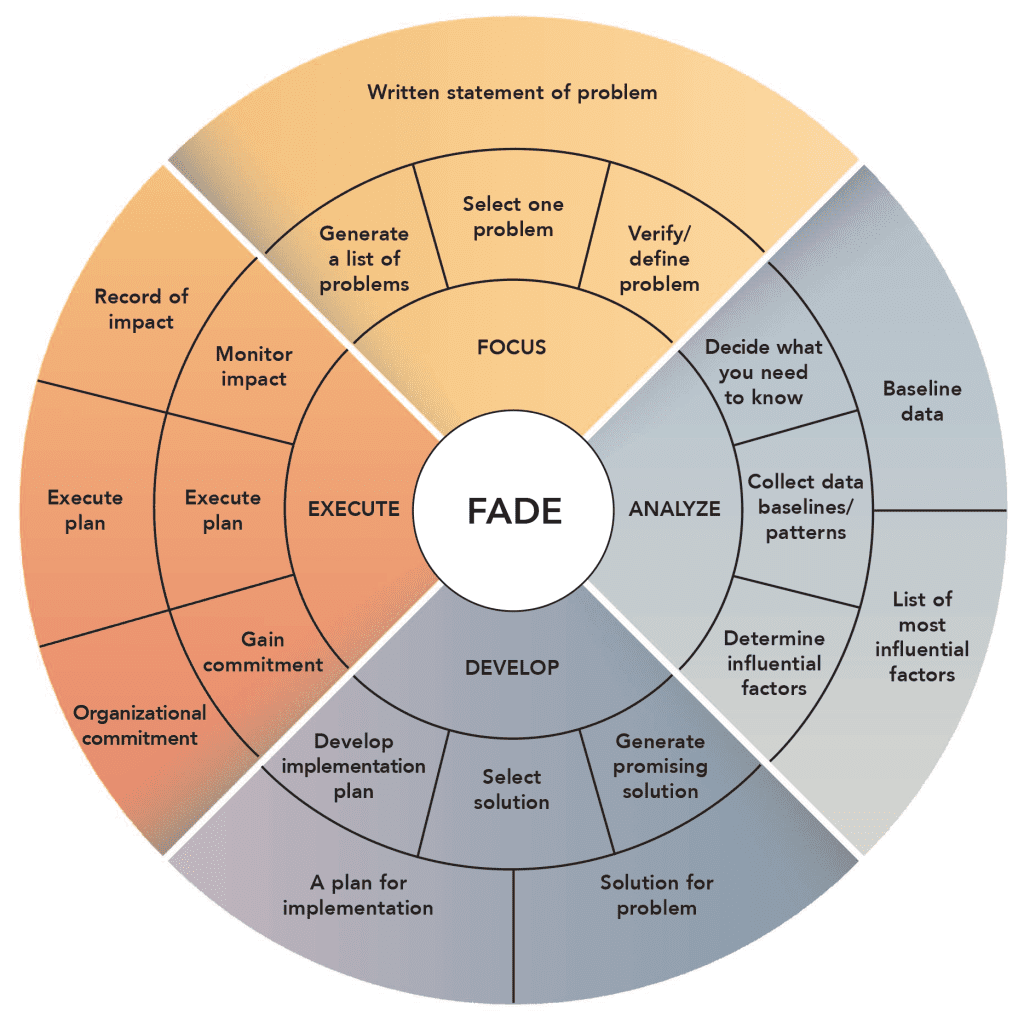
An evidence-based, quality-improvement project aimed at increasing the number of ASCVD risk screenings in adult patients with T2DM helped improve providers’ actions post-screening in those at moderate to high risk. The project team used the Josie King Foundation’s FADE (focus, analyze, develop, and execute) model at each touchpoint and as needed to address ongoing barriers such as EHR technical issues. The project increased the number of screenings and prompted providers to collaborate with patients to improve their health.
A simple tool
To understand whether the ASCVD risk score tool recommendation would benefit adult patients with T2DM, a primary care clinic implemented a 15-week quality-improvement (QI) project. The project’s goals included increasing adult ASCVD assessments and risk screening rates by 10%, providing education, engaging patients in actively participating in their care, and improving provider decisions related to treatment and diet recommendations in patients deemed at moderate to high risk. For any lipid panel result, the EHR automatically calculated an ASCVD score, which the provider could pull into their notes.
Before project implementation, the QI team asked providers if they currently use the tool. Most didn’t know that the EHR had an embedded risk score tool, which led to missed stratification and education opportunities and increased the chances of inappropriate or no treatment.
A study by Das and colleagues noted the missed treatment opportunities related to underuse of the ASCVD risk score calculator. Of the 89% of study participants who received an ASCVD risk assessment, over 99% had ASCVD risk factors; over 66% of participants <40 years of age had risk factors. Only 30% of all study participants met the 2018 American Diabetes Association (ADA) low-density lipoprotein (LDL) target of <100 mg/dL. For patients ≥40 years of age, 91.5% with at-risk ASCVD scoring didn’t have an LDL result. Of the patients <40 years of age, 64% had no high-density lipoprotein (HDL) lab results noted in the EHR.
The FADE model, with its succinct cyclic process steps that closely resemble the Plan-Do-Study-Act model, best supported the clinic’s QI project. The FADE model includes focus and analysis to appropriately guide the QI process and help achieve the proposed, measurable outcome of increasing ASCVD risk stratification in adults with T2DM. During implementation, the project team completed 15 FADE model cycles, including ongoing touchpoints with the clinic providers and information and analytics services team members to discuss positive outcomes and identify barriers to the project workflow. (See FADE model.)
FADE model
The Josie King Foundation’s FADE (focus, analyze develop, and execute) model helped guide the quality improvement project process.
Source: Patient safety module series used with permission from Duke University. ©Duke University 2023.
Implementation plan
The QI project team established a baseline of 0 ASCVD risk scores pulled into a provider clinic note. After education with providers and clinic staff, the project began, with weekly updates to capture the number of ASCVD risk scores in the provider note. The team also captured the “met” or “unmet” clinic health system’s diabetes registry metrics for blood pressure (<140/90 mmHg), HbA1c (<8%), HbA1c monitoring, nephropathy monitoring, statin therapy, and eye exam. (Note that the American Heart Association [AHA]/American College of Cardiology’s [ACC] current HbA1c goal is <6.5%). To address ongoing COVID-19 surges, the team established alternate go-live dates.
Results
During the project, the clinic saw 119 adult patients with T2DM and lipid panel results either in-person or during a virtual visit. The ASCVD risk scores included in a provider note rose by 9.24%, slightly below the 10% goal. The health system’s weighted composite targets for blood pressure and statin therapy were 79.93% and 87%, respectively. The results fell below the targets at 71.55% for blood pressure and 53.21% for statin therapy.
Although targeted outcomes weren’t reached, bringing awareness of the EHR risk score tool and the project purpose to the clinic staff sparked conversations between patients and providers. Using the embedded ASCVD risk score tool, providers engaged patients in healthcare discussions and shared decision-making to improve patients’ health and well-being, especially regarding individual risk levels.
Limitations and facilitators
Providers encountered a few challenges related to software limitations. For example, if they attempted to pull in a risk score related to lipid panel results from a previous EHR encounter, the risk score wouldn’t populate in the note, which created frustration and jeopardized buy-in. Another limitation of the software required providers to go back to their notes to retrieve risk scores related to lipid panels drawn the same day as the visit. The lack of a visual reminder during the visit delayed patient conversations until a follow-up call or a future virtual or clinic visit. In addition, only the lead clinic provider and two residents on the original project team remained at the end of implementation after other residents had completed their rotations and moved to other sites.
In addition to the visual risk score, which functioned as a reminder to providers to initiate patient conversation, the AHA’s Get with the Guideline® Stroke Gold Certification and the ADA/AHA Know Diabetes by Heart™ Silver Certification program ignited interest in the project. These facilitators aided project progress, even in the face of unexpected challenges and noted limitations.
Implications for patients
In addition to improving patient health and well-being, involving patients in discussions about risks and participating in shared decision making also supported improved self-management skills to reduce cardiovascular risk. Nutrition and exercise discussions prompted by the ASCVD risk score tool increased patient and family participation in healthy lifestyle changes. Engaging patients not only improves the chances of decreasing their future out-of-pocket costs for health management but also reduces the risks of morbidity and mortality from CVD and strokes.
Implications for nursing practice
The project and outcomes supported a firm understanding of the need for nurses and nursing leaders to help drive patient outcome improvements with interprofessional care team approaches. It also aided collaboration among nurses and providers during patient clinic visits for improved patient education using the visible ASCVD risk score results. With most, if not all, data needed for scoring already documented in a patient’s chart, nurses can proactively enter information into an online or mobile calculator if the scoring tool isn’t currently embedded in the EHR. If any data aren’t available during the clinic visit, nurses can recommend that the provider order lab tests. However, this might require retroactive scoring.
Historically, nurse-provided patient education is provider-directed. However, with providers initiating collaborations with patients using the visible ASCVD risk score results, nurses can become more involved in patient education as part of the interprofessional care team during and after appointments. Post-appointment actions include follow-up phone calls or video/clinic visits for treatment changes and education after a retroactive risk score result for patients at medium to high risk.
Using external educational and guidance resources such as those provided by the ADA/AHA Know Diabetes by Heart™ Silver Certification program, together with discussions on the ASCVD risk scores, can help streamline appropriate lifestyle change recommendations and improve goal setting and target outcomes for patients. The project’s hospital system was already enrolled in the nurse-driven AHA Get with the Guidelines™ Gold Certification program, which works appropriately in conjunction with the ADA/AHA program. Lippincott NursingCenter described the ASCVD risk scores and resulting patient discussions as significant and included them in their summary of the ACC/AHA 2019 guidelines for nursing collaboration with interventional approaches.
Implications for healthcare systems
A literature review, conducted in preparation for the QI project, indicated that an EHR-embedded or other appropriate risk score tool can aid healthcare system efficiency. In addition, nurse, provider, and patient collaborations related to improved medical support and individualized lifestyle and treatment changes help decrease costs for healthcare systems and patients. Increasing Centers for Medicare & Medicaid Services reimbursements by improving accountable care organization metric targets for primary care provider clinics also can have a positive future impact. This project highlighted how simple EHR tools (and manual applications) can support metric target outcomes to improve those reimbursements.
Collaborations for health
Before implementing this project in other hospital systems or ambulatory clinics, test criteria discernment within reporting portals to reduce gaps and barriers and ensure availability of all needed data and outcomes for the appropriate patient population. An EHR risk score tool technical build should include low, moderate, and high ASCVD risk scores within a provider note to visually prompt providers to address individual patient needs and guide decisions by risk level. In addition, the project team should collect at least 6 months of data post-implementation to ensure significant metrics.
QI projects aid healthcare improvement. Primary care ambulatory providers serve as the first line of defense against serious health issues, and a simple embedded EHR tool can help guide healthcare decisions. Discussing risk scores with patients engages them in shared decision-making to decrease mortality and morbidity and reduce out-of-pocket healthcare costs. In addition to reducing long-term risks and increasing hospital reimbursement, collaboration aligns with worldwide initiatives and recommendations to continue improving individual and population health.
Victoria Bhardwaj works at the Medical University of South Carolina (MUSC) in Charleston, where she’s a Program Manager II – Care Transitions and a co-chair with Enterprise Readmissions Reduction Sustainability.
American Nurse Journal. 2023; 18(10). Doi: 10.51256/ANJ102340
References
Agency for Healthcare Research and Quality. Health Literacy Universal Precautions Toolkit, 2nd Edition: Plan-Do-Study-Act (PDSA) directions and examples. September 2020. ahrq.gov/health-literacy/improve/precautions/tool2b.html
Agency for Healthcare Research and Quality. Section 4: Ways to approach the quality improvement process. January 2020. ahrq.gov/cahps/quality-improvement/improvement-guide/4-approach-qi-process/index.html
American College of Cardiology. ASCVD risk estimator plus. tools.acc.org/ascvd-risk-estimator-plus
American College of Cardiology. Diabetes outcomes strongly influenced by income and education. American College of Cardiology. August 1, 2016 cardiosmart.org/news/2016/8/diabetes-outcomes-strongly-influenced-by-income-and-education
American Heart Association. Get with the Guidelines® – Stroke recognition overview. August 10, 2022. heart.org/en/professional/quality-improvement/get-with-the-guidelines/get-with-the-guidelines-stroke/recognition-from-get-with-the-guidelines-stroke
Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;74(10):e177-232. doi:10.1016/j.jacc.2019.03.010
ASCVD Risk Estimator Plus. apps.apple.com/us/app/ascvd-risk-estimator-plus/id808875968
Centers for Disease Control and Prevention. Healthy People 2020. December 14, 2020. cdc.gov/nchs/healthy_people/hp2020.htm
Centers for Disease Control and Prevention. National diabetes statistics report. June 29, 2022. cdc.gov/diabetes/library/features/diabetes-stat-report.html
Das AK, Saboo B, Unnikrishnan AG. Current practices and gaps in management of dyslipidemia in type 2 diabetes mellitus (T2DM) in accordance with American Diabetes Association (ADA) guidelines: A subset analysis from a real-world, cross-sectional observational study (LEADD study). Diabetes Metab Syndr Obes. 2021;14:2693-2700. doi:10.2147/DMSO.S294842
Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 suppl 2):S49-73. doi:10.1161/01.cir.0000437741.48606.98
Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines. Circulation. 2019;139(25):e1046-81. doi:10.1161/CIR.0000000000000624
Hong SM, Choi YM, Hong E-G. Comparison of the ASCVD and UK prospective diabetes study risk engine with carotid intima media thickness and brachial-ankle pulse wave velocity. Diabetes. 2019;68(suppl 1):436-P. diabetesjournals.org/diabetes/article/68/Supplement_1/436-P/60397/436-P-Comparison-of-the-ASCVD-and-UK-Prospective
Josie King Foundation. FADE model in action. josieking.org/patientsafety/module_a/methods/fade_model_action.html
KnowDiabetesByHeart. Clinical practice and health system change guide: Principles of diabetes and cardiovascular management for ambulatory care settings. American Diabetes Association and American Heart Association. knowdiabetesbyheart.org/wp-content/uploads/2021/01/KDBH-Clinical-Practice-Guide-Booklet_Ambulator.pdf
Lippincott NursingCenter. Primary prevention of cardiovascular disease. February 2020. nursingcenter.com/getattachment/Clinical-Resources/Guideline-Summaries/Primary-Prevention-of-Cardiovascular-Disease/Guideline-Summary_Primary-Prevention-of-Heart-Disease_January-2020.pdf.aspx
Ngo-Metzger Q. U.S. preventive services task force abnormal blood glucose screening. Behavioral interventions. Agency for Healthcare Research and Quality. 2017. https://www.healthypeople.gov/sites/default/files/HP2020%20Spotlight%20on%20Health%20Diabetes%20Webinar.pdf
Yang J, Zhao Y, Ren Y, et al. Identification of undiagnosed diabetes mellitus and associated alternation of predicted ASCVD risk using Chinese and U.S. risk calculators. Diabetes. 2020;69(suppl 1):1486-P. doi:10.2337/db20-1486-P
Key words: atherosclerotic cardiovascular disease, cardiovascular disease, type 2 diabetes, diabetes risk stratification