Awareness and assessment are keys to getting victims the help they need.
Takeaways:
- The effects of strangulation can be delayed.
- Nonfatal strangulation victims are at increased risk for homicide after the first incident.
- Accurate assessment of strangulation victims is crucial to decreasing postincident health impacts.
According to the Centers for Disease Control and Prevention (CDC), between 2003 and 2014, 55.3% of female homicide victims in the United States were the result of intimate partner violence (IPV). The CDC also reports that nearly one in four adult women and approximately one in seven adult men report having experienced severe physical violence, including strangulation, from an intimate partner in their lifetime. According to the 2015 National Intimate Partner and Sexual Violence Survey (NISVS), 21.4% of female respondents have experienced severe physical violence in their lifetime.
Strangulation is a violent and sometimes deadly act. (See Strangulation facts.) Many people believe that strangulation leaves obvious evidence, but visible signs may not occur for hours to days after the incident. Victims frequently don’t report strangulation because they’re afraid and they don’t think they’ll be believed if no physical evidence exists. Your interviewing techniques and assessment skills can help detect strangulation in patients and identify those at risk for strangulation.
Strangulation is the compression of anatomic neck structures leading to a reduction of blood flow to or from the brain that results in injury or death. Using the average handshake at 80 to 100 pounds of pressure as comparison:
- a victim’s jugular veins will occlude when a perpetrator applies only 4 pounds of pressure
- occlusion of the carotid arteries occurs with 5 to 11 pounds of pressure
- a perpetrator applying 33 pounds of pressure to the victim’s trachea will cause it to collapse.
Strangulation signs and symptoms may not be visible during the initial victim assessment. According to Zilkens and colleagues, approximately 50% of strangulation victims will have no visible injuries, and some survivors may not even recall the strangulation incident because of cerebral hypoxia during the assault.
Risk factors
According to Glass and colleagues, victims who previously experienced a nonfatal strangulation (NFS) are six times more likely to be victims of attempted homicide and seven times more likely to die by homicide than those who haven’t experienced NFS. After a victim experiences one episode of NFS, his or her chance of experiencing recurrent strangulation episodes increases. In addition, according to Messing and colleagues, victims of multiple strangulations are at a greater risk for miscarriages associated with the abuse, loss of consciousness, IPV injuries, and homicide.
Sexual assault increases the risk for strangulation. Based on research by Zilkens and colleagues, the risk of being strangled is approximately five times higher for women who’ve been sexually assaulted by an intimate partner than those assaulted by a stranger. More than 33% of NFSs occur in women 30 to 39 years old who were sexually assaulted by an intimate partner. Women who experience IPV that involves strangulation are at high risk for death. Other factors associated with NFS during sexual assaults include denial of freedom, verbal threats, assault occurring in the victim’s home, and use of blunt force.
Signs and symptoms
An NFS can range from mild and transitory to serious and life-threatening, and it may result in injuries such as carotid artery dissection, thrombosis, or embolism, as well as bruising or fracture of the larynx, hyoid bone, tracheal rings, or thyroid cartilage. Subjective data indicating possible strangulation include:
- neck or throat pain
- discomfort or difficulty swallowing or talking
- vocal changes
- shortness of breath
- loss of consciousness
- memory loss
- dizziness
- feeling faint
- blurry vision
- involuntary urination or defecation
- tinnitus.
You should suspect NFS if a victim of IPV exhibits neurologic symptoms such as seizures, stroke symptoms, concentration and recall difficulties, or agitation. Physical signs that may indicate strangulation include:
- linear abrasions
- bruising on the upper neck, chin, or face
- subconjunctival hemorrhage
- conjunctivae petechia
- neck swelling
- neck tenderness upon palpation.
Forty percent of NFS victims will present to healthcare professionals with a neck injury, voice loss or vocal changes, and/or difficulty breathing. However, they may not exhibit signs or symptoms of strangulation until 24 to 36 hours after the incident. Laryngeal edema may take up to 36 hours to occur, delaying airway obstruction and respiratory compromise.
Screening
Organizations should develop IPV and strangulation policies for screening/assessment, evaluation, documentation, and discharge planning to help nurses in early detection and treatment. If your organization doesn’t have such policies, advocate for and help implement them.
Ask the right questions
When assessing a victim of IPV, ask if any form of strangulation has occurred and use wording (such as squeezed neck, choked, and choked off) that ensures that he or she understands what you’re asking. Structure questions about strangulation according to methods that could be used, such as “Has anyone squeezed or pressed against your throat until you couldn’t breathe, or you passed out? Has anyone wrapped his or her arm around your neck from behind and pressed against your throat?”
In addition, ask how many times the victim has been strangled and help him or her break down the frequency into the number of strangulations in each incident and the number of times he or she has been strangled by present and past partners. Inform victims who’ve been strangled in the past 24 to 48 hours that they may experience delayed responses, including airway compromise or neurologic injuries. And remember that skin tone variations (such as darker tones) can hinder your identification of physical signs of strangulation.
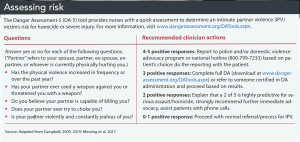
Links above: www.dangerassessment.org/DATools.aspx, www.dangerassessment.org/DATools.aspx
Use a screening tool
Currently, no standard test, tool, or indicator exists to evaluate specifically for strangulation, and no national or international organizations have recommended one tool over another. However, one tool frequently discussed in the literature is the Danger Assessment (DA) tool, which is designed to detect the risk of deadly violence and extreme danger in an abusive intimate relationship. Research indicates that the DA tool has the highest Cronbach alpha (α=.66) compared to other lethality assessment tools. It’s available in a short version that includes only five questions (DA-5) to aid in identifying individuals at high risk for homicide or severe injury by an intimate partner. (See Assessing risk.) The full version can be administered if the results of the DA-5 raise concerns.
The full DA tool includes use of a calendar that allows victims to record the types of IPV injuries they’ve experienced and their frequency. The calendar raises the victim’s awareness of the abuse and decreases his or her denial of it. The second part of the tool includes 20 items requiring yes or no responses. The DA is scored by adding the number of “yes” items; the more “yes” answers, the greater the risk of severe repeated or lethal violence. The full DA tool also is available ias an app (which includes the weighted scoring algorithm), available at myplanapp.org.
The DA website also includes additional resources to help nurses and other healthcare professionals increase their knowledge of strangulation and assessment skills, and it also offers certification. Once certified, no renewals are required. Training and certification are valuable and affordable but not necessary. However, healthcare professionals in settings such as emergency departments that frequently encounter IPV victims may want to consider certification. At a minimum, healthcare providers should incorporate the DA-5 for patients who’ve been involved in a suspected or revealed IPV incident. (See Resources.)
Resources
Access these resources for more information about intimate partner violence and strangulation.
This free screening tool is available in a variety of languages, as well as a version for use with women who are immigrants. The site also offers free training and certification for healthcare professionals.
Family Justice Center Alliance (888-511-3522)
This research center, clearinghouse, and national affiliation organization for family justice centers serves victims of domestic violence, sexual assault, human trafficking, elder abuse, and child abuse.
International Association of Forensic Nurses
The association offers a Non-Fatal Strangulation Documentation Toolkit to help nurses develop policies for their organizations.
Training Institute on Strangulation Prevention
This organization offers free strangulation prevention resources, training, and certification for healthcare professionals.
Nursing implications
Understanding the prevalence of strangulation, its varying degrees of severity, and delayed symptom onset can help you identify this form of IPV even when no obvious signs are evident during patient assessment. If you suspect IPV has occurred, take an unhurried approach to continuing the assessment and build trust with the patient as you ask relevant questions about abuse and injuries. Emphasize that strangulation symptoms may be delayed and that the patient should report late or worsening symptoms immediately.
Review your organization’s current policies and procedures related to IPV in general and strangulation in specific so that you’re familiar with treatment and reporting processes. If your organization doesn’t have any relevant policies, work with leadership to develop and implement them. The International Association of Forensic Nurses has a model policy toolkit to help organizations develop policies, which should include a process for connecting victims with resources (such as social workers and community services) that can help them develop a safety plan for the future.
With increased education and community partnerships, nurses are in a power position when it comes to identifying IPV and strangulation risk factors and decreasing adverse effects. These partnerships can help combat this silent and deadly act of violence.
The authors are assistant professors at the University of Louisiana at Lafayette College of Nursing and Allied Health Professions.
References
Campbell JC, Webster DW, Glass N. The danger assessment: Validation of a lethality risk assessment instrument for intimate partner femicide. J Interpers Violence. 2009;24(4):653-74.
Campbell JC. Danger Assessment. Update 2019. www.dangerassessment.org/uploads/DA_NewScoring_2019.pdf.
Centers for Disease Control and Prevention. Violence prevention: Preventing intimate partner violence. February 26, 2019. cdc.gov/violenceprevention/intimatepartnerviolence/consequences.html
Dunn RJ, Lopez RA. Strangulation injuries. StatPearls. July 3, 2019. ncbi.nlm.nih.gov/books/NBK459192
Glass N, Laughon K, Campbell J, et al. Non-fatal strangulation is an important risk factor for homicide of women. J Emerg Med. 2008;35(3):329-35.
Hume K. Strangulation, Risk, and Lethality in Domestic Violence. Colorado Department of Public Safety. August 11, 2017. files.constantcontact.com/bfd9ce68401/aa67220e-fce5-4adb-b073-73d97a3d20a0.pdf
Mcquown C, Frey J, Steer S, et al. Prevalence of strangulation in survivors of sexual assault and domestic violence. Am J Emerg Med. 2016;34(7):1281-5.
Messing JT, Patch M, Wilson JS, Kelen GD, Campbell J. Differentiating among attempted, completed, and multiple nonfatal strangulation in women experiencing intimate partner violence. Womens Health Issues. 2018;28(1):104-11.
Messing JT, Campbell JC, Snider C. Validation and adaptation of the Danger Assessment-5: A brief intimate partner violence risk assessment. J Adv Nurs. 2017;73(12):3220-30.
Petrosky E, Blair JM, Betz CJ, Fowler KA, Jack SPD, Lyons BH. Racial and ethnic differences in homicides of adult women and the role of intimate partner violence—United States, 2003-2014. MMWR Morb Mortal Wkly Rep. 2017;66(28):741-6.
Roehl J, O’Sullivan C, Webster D, Campbell J. Intimate Partner Violence Risk Assessment Validation Study, Final Report. U.S. Department of Justice. May 2005. ncjrs.gov/pdffiles1/nij/grants/209731.pdf
Smith SG, Zhang X, Basile KC, et al. National Intimate Partner and Sexual Violence Survey: 2015 data brief. Centers for Disease Control and Prevention. cdc.gov/violenceprevention/datasources/nisvs/2015NISVSdatabrief.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fviolenceprevention%2Fnisvs%2F2015NISVSdatabrief.html
Sorenson SB, Joshi M, Sivitz E. A systematic review of the epidemiology of nonfatal strangulation, a human rights and health concern. Am J Public Health. 2014;104(11):e54-61.
Washington State Coalition Against Domestic Violence.New data from the National Intimate Partner & Sexual Violence Survey (NISVS). June 28, 2018. wscadv.org/news/new-data-from-the-national-intimate-partner-sexual-violence-survey-nisvs
Zilkens RR, Phillips MA, Kelly MC, Mukhtar SA, Semmens JB, Smith DA. Non-fatal strangulation in sexual assault: A study of clinical and assault characteristics highlighting the role of intimate partner violence. J Forensic Leg Med. 2016;43:1-7.



















2 Comments.
It’s scary to learn that one in four women and be in seven men has experienced extreme physical violence including strangulations from their partners. Well, you made a pretty good point that victims who may have experienced non-fatal strangulations are more likely to become victims of attempted homicide. Well, if I were an investigator that handles this type of case, I’ll probably work with an expert that specializes in strangulation because his findings could be used as evidence in court.
Excellent. I was strangled once. Another sign that I had was petechiae not only in my eyes but all over my face. It looked like a rash. I pretended that is what it was. I was shocked and embarrassed that he did this to me, so I lied about it.