What’s a nurse to do without an asthma educator?
CNE 1.5 contact Hours
Learning Objectives
1. Identify triggers associated with asthma.
2. Discuss medications used to manage asthma.
3. Describe strategies for educating children with asthma and their families and caregivers.
The authors and planners of this CNE activity have disclosed no relevant financial relationships with any commercial companies pertaining to this activity. See the last page of the article to learn how to earn CNE credit.
Expiration: 8/1/23
Takeaways
- Asthma is not curable, but it is controllable, and requires disease knowledge and understanding, which is gained through proper education.
- In the absence of an asthma educator, nurses need a general understanding of the basics of asthma to provide patient education.
- Medication administration is a major factor in asthma control.
Asthma, a chronic condition that leads to significant morbidity and mortality, affects 24.6 million people in the United States; 6.2 million of those are children. These numbers make asthma control a top priority for healthcare providers. According to the National Heart, Lung, and Blood Institute’s National Asthma Education and Prevention Program Expert Panel Report 3 (EPR-3), Guidelines for the Diagnosis and Management of Asthma, comprehensive patient, family, and community education is crucial to disease management.
In inpatient settings, asthma educators typically teach children and their families how to manage their disease; however, if no asthma educator is present, nurses may take on this role. To ensure no important information is missed, nurses should be familiar with EPR-3 guidelines, and they should be alert to other teachable moments that might arise during patient education.
Asthma basics
Asthma is characterized by airflow reduction from bronchoconstriction, airway inflammation, thickened mucus secretions, and airway hyper-responsiveness, which can reverse spontaneously or with treatment. Signs and symptoms (coughing, wheezing, dyspnea, chest tightness, and increased sputum production) vary depending on disease severity, which is classified as intermittent or persistent. Persistent asthma is further divided into three categories: mild, moderate, or severe. Asthma is considered controlled when symptoms no longer are present. (See Get control.)
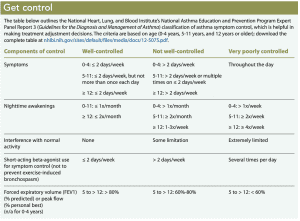
Treatment is based on the level of symptom control, which is determined by asking patients and families these questions: How often do symptoms occur? Do symptoms occur at night? How often are rescue medications used? Do symptoms affect normal activity? And for patients old enough to use a peak flow meter (PFM), where do results fall in their personal best? (See What’s best?)
Symptom and trigger identification
Early symptom and aggravating factor (trigger) identification can aid asthma control. Ask patients and their families what symptoms patients experience, what steps they take to alleviate symptoms, and how long they wait before starting treatment. Help patients and families determine if symptoms have a pattern (for example, worse at night or occur during certain seasons) and if they’re continual or episodic.
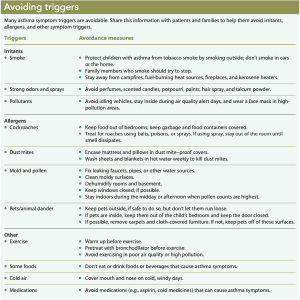
Exposure to triggers (which are grouped as irritants, allergens, and others) can cause lung inflammation; continual contact worsens symptoms. Some triggers are avoidable, but others aren’t. Help patients and families learn to identify their triggers and review how to avoid them. (See Avoiding triggers.)
Environmental irritants
Environmental irritants—including smoke (from tobacco, burning leaves or trash, forest and campfires, and woodburning stoves), strong odors (from perfume, scented candles, potpourri, hair spray, paint, lotions, and household cleaners), and outdoor pollutants (car and bus exhaust, ozone, factory fumes, and agricultural sprays)—are found everywhere.
Children who are exposed to secondhand tobacco smoke (and also thirdhand from residual smoke on people, clothes, or furniture fabric, or in cars, walls, and carpeting) are more likely to be hospitalized with asthma exacerbations and struggle to gain control of their symptoms. For example, emergency departments frequently see spikes in asthma admissions after the first cold spell, when fireplaces or kerosene heaters are being used.
A peak flow meter is used to measure how fast a patient can forcefully exhale air from the chest. The result helps determine if asthma symptoms are under control and when to start rescue medications. Control is measured in green, yellow, or red zones based on the patient’s personal best effort, which is established by having the patient blow into the device twice a day over a 2-week, symptom-free period.
- Green zone is 80% to 100% of personal best—no treatment necessary.
- Yellow zone is 50% to 80% of personal best—start rescue medications and monitor for an acute exacerbation.
- Red zone is below 50% of personal best—signals an emergency; rescue medications should be given and immediate medical care should be sought.
Allergens
Indoor allergens include roaches, dust mites, mold, and pets. Outdoor allergens include pollen and mold. Review patients’ possible exposure to allergens, including activities over the last several days to identify triggers.
Other triggers
Other asthma triggers include exercise, strong emotional reactions that trigger heavy breathing (such as laughing or crying), weather changes (high humidity or cold, dry air), food allergies, viruses, and gastroesophageal reflux disease.
Exercise-induced bronchospasm (transient respiratory distress) symptoms can occur during or after exercise and affect people with or without chronic asthma. Exercise keeps the lungs and body healthy and is part of routine asthma care, so patients shouldn’t avoid it. Teach patients and families that they can decrease symptoms during exercise by avoiding allergens and pollutants, warming up before exercise, breathing through the nose rather than the mouth, choosing activities (such as swimming) less likely to trigger asthma, pacing activity based on symptoms, and gradually increasing as tolerated. Exercise enhances physical conditioning, which improves lung health (by building muscles, increasing lung capacity, reducing inflammation, and increasing endurance) so the lungs can better tolerate activities that would otherwise leave patients winded. For many patients, pretreatment with a short-acting bronchodilator shortly before exercise controls symptoms. If this doesn’t help, the family should speak with the child’s healthcare provider for long-term therapies.
For patients and families who aren’t sure what triggers their asthma symptoms, recommend that they keep a symptom diary. They can use the diary to track symptoms, events occurring when symptoms began, treatments used, and response achieved. Sharing the diary with the primary healthcare provider can help identify trends, making it easier to recognize triggers.
Medications
Asthma medications fall into two categories: rescue and controller. Rapid symptom identification and management is the focus in the hospital setting, where care and management are dictated by symptom severity. When the exacerbation is under control, focus shifts to returning the patient to baseline symptom maintenance. You can help patients and their families understand how to use their medications.
Rescue medications
Rescue medications provide quick bronchoconstriction and airway hyper-responsiveness relief. They’re taken when symptoms occur, not for daily control. Evaluate patients for poor symptom control if they report using rescue medications daily. Instruct patients and families to contact their healthcare provider if they need a rescue treatment more than every 4 hours.
Rescue medications fall into three categories: inhaled short-acting beta-agonists (SABAs), anticholinergics, and systemic corticosteroids.
SABAS. SABAs (including albuterol and levalbuterol) are inhaled through a metered dose inhaler (MDI) or nebulized solution. They relax constricted airway muscles, leading to bronchodilation. SABAS usually are the first choice for acute exacerbations because of their quick onset and short duration of action. The provider should prescribe a rescue inhaler before discharge. Teach the patient and family how to use the inhaler, and ask for a return demonstration to ensure they understand.
Anticholinergics. Ipratropium bromide is the only anticholinergic approved to relieve bronchospasm; it can be combined with albuterol for moderate to severe asthma exacerbations. Provide inhaler use instruction, and ask the patient to perform a return demonstration.
Systemic corticosteroids. Systemic corticosteroids (for example, prednisone, prednisolone, or methylprednisolone) reduce inflammation and increase SABA effectiveness. These medications usually are started on admission and continued for 3 to 5 days after discharge depending on hospital length of stay. Focus your teaching on taking the medication as prescribed and preventing short-term (such as facial flushing and weight gain) and long-term (such as fractures and delayed growth) side effects. For example, taking short “bursts” of systemic corticosteroids and properly using controller medications can decrease the need for these medications and help alleviate some long-term side effects.
Controller medications
Controller medications fall into five categories: inhaled corticosteroids (ICSs), inhaled long-acting bronchodilators, leukotriene modifiers, theophylline, and immunomodulators. ICSs are the most commonly prescribed medications at discharge. Other controller medications (such as montelukast and shots) may be explored at a follow-up appointment with the patient’s primary care provider or an asthma specialist.
Common ICSs are beclomethasone, budesonide, flunisolide, fluticasone, and triamcinolone acetonide. The recommended dosage is based on symptom severity. Due to the mechanism of action, all ICSs are meant to be taken daily, even if no symptoms exist. Regular use reduces asthma symptoms, frequency of acute episodes, and use of medical resources.
Many patients don’t take ICSs as prescribed because they mistakenly believe these medications have the same side effects as anabolic steroids (hair loss, liver and kidney disease, increased aggression). Explain the difference between the medications to encourage adherence.
Focus patient education on how ICSs reduce lung swelling, leading to better symptom control and improved quality of life, and emphasize the importance of following the daily dose and schedule. A common side effect of ICSs is thrush. Instruct patients to rinse their mouth with water after each dose to reduce risk.
Encourage patients and families to talk about their fears, frustrations, or doubts with the medication or administration process, and then follow up with reassurance, answers to their questions, and resources for additional information.
Devices and administration techniques
Asthma medications can be given via nebulizer, MDI, breath-actuated device, or dry powdered inhaler (DPI). When a medication or its administration device aren’t properly used, the medication may fail and lead patients and families to think it doesn’t work. Evaluate administration techniques so you can correct errors.
Nebulizers
Nebulizers with a facemask are commonly used in children under 5 years old and in those with cognitive impairment to ensure proper medication delivery. The face mask should fit snuggly over the child’s mouth and nose; instruct the patient to breathe normally. Instruct patients more than 5 years old who use a mouthpiece nebulizer to:
- place it in the mouth between the teeth with lips closed tightly
- breathe in through the mouth rather than the nose.
Nebulized treatment is less effective when administered “blowby” (the medication is blown in front of the face without the use of a facemask or mouthpiece). However, this technique may be used in children between 1 and 3 years old who fight the mask.
MDIs
Patients using non-breath–activated MDIs should use a valve holding chamber (spacer) to increase medication efficacy and reduce thrush risk. A spacer with a facemask should be used for children under 5 years old. Instruct the patient to:
- shake the cannister vigorously for 5 seconds and place it into the spacer
- depress one puff
- take six to eight breaths
- wait 1 minute and repeat as prescribed.
For a spacer with a mouthpiece, instruct the patient to:
- shake the cannister and place it in the end of the spacer
- breathe all the way out
- place the mouthpiece in the mouth with upper teeth on top, tongue below, and lips closed tight
- depress the cannister while taking a slow deep breath
- hold the breath for 10 seconds
- wait 1 minute and repeat as prescribed.
Breath-actuated devices and DPIs
A breath-actuated device releases medication as the patient inhales and doesn’t require a spacer. DPIs also are breath actuated and require the patient to be able to take a deep, fast breath to receive the medication. Demonstrate the correct technique for the patient and family, and then ask the patient to perform a return demonstration.
Asthma action plan
The Joint Commission’s Children’s Asthma Care Core Measures require that an asthma action plan (AAP), developed in collaboration with the patient, be completed before hospital discharge. The plan should include triggers and symptoms. Symptoms are classified in green, yellow, and red zones to indicate severity. Controller medications are listed in the green zone, indicating symptom control; rescue medications with dosages are listed in the yellow and red zones based on symptom severity.
Review the AAP with the patient and family, and send it home with them. Schedule a follow-up appointment with the child’s primary care provider or asthma specialist within 2 to 3 days of discharge. If discharge occurs when the provider’s office is closed, instruct the patient and family to schedule an appointment as soon as possible. Encourage them to take the AAP to the appointment to facilitate a conversation about asthma care and how to respond to future exacerbations.
If the AAP is signed by a provider, school nurses can use it to administer medications if necessary. The plan also can include direction for the child to carry a rescue inhaler for self-administration in the event of an exacerbation. A copy of the AAP should be given to everyone who cares for the child (for example, other family members and daycare providers) to ensure rapid and appropriate response to an exacerbation.
Talk with patients and families about the importance of following the AAP to ensure asthma control, ask if they have any concerns or questions, and assess for potential nonadherence. Common reasons for not following the AAP include a lack of understanding about the medications prescribed (effectiveness, action, purpose, and side effects), denial or under-recognition of symptom severity, feeling overwhelmed by daily treatments, inability to afford medications, and poor recognition of early symptoms. Remain nonjudgmental, answer questions, and provide access to additional resources.
Be prepared
Asthma isn’t curable, but it is controllable. Nurses must be prepared to provide asthma education in the absence of a designated asthma educator to satisfy The Joint Commission’s core measures and to prepare patients and families for appropriate asthma management. When you understand the asthma basics, you can provide appropriate education to equip patients and families with the knowledge they need.
Casey L. Norris is an assistant professor at Lincoln Memorial University in Knoxville (Cedar Bluff), Tennessee. Linda Gibson-Young is an associate professor at Auburn University School of Nursing in Auburn, Alabama.
References
American Academy of Allergy Asthma & Immunology. Asthma triggers and management. aaaai.org/conditions-and-treatments/library/asthma-library/asthma-triggers-and-management.
Arnold CM, Bixenstine PJ, Cheng TL, Tschudy MM. Concordance among children, caregivers, and clinicians on barriers to controller medication use. J Asthma. 2018;55(12):1352-61.
Braido F, Chrystyn H, Baiardini I, et al. “Trying but failing”—The role of inhaler technique and mode of delivery in respiratory medication adherence. J Allergy Clin Immunol Pract. 2016;4(5):823-32.
Clayton S. Adherence to asthma medication. Nurse Prescribing. 2014;12(2):68-74.
Hekking PP, Amelink M, Wener RR, Bouvy ML, Bel EH. Comorbidities in difficult-to-control asthma. J Allergy Clin Immunol Pract. 2018;6(1):108-13.
Hossny E, Rosario N, Wah Lee B, et al. The use of inhaled corticosteroids in pediatric asthma: Update. World Allergy Organ J. 2016;9:26.
Hui RWH. Inhaled corticosteroid-phobia and childhood asthma: Current understanding and management implications. Paediatr Respir Rev. 2020;33:62-6.
Janssens T, Harver A. Effects of symptom perception interventions on trigger identification and quality of life in children with asthma. Pulm Med. 2015:825137. hindawi.com/journals/pm/2015/825137
Kenyon CC, Auger KA, Adams SA, Loechtenfeldt A, Moses JM. Improving asthma care in the hospital: An overview of treatments and quality improvement interventions for children hospitalized for status asthmaticus. Curr Treat Options Pediatr. 2015;1(1):100-12.
Mavissakalian M, Brady S. The current state of biologic therapies for treatment of refractory asthma. [published online ahead of print January 24, 2020]. Clin Rev Allergy Immunol.
National Asthma Education and Prevention Program. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. National Heart, Lung, and Blood Institute. 2007. ncbi.nlm.nih.gov/books/NBK7232
Nurmagambetov T, Kuwahara R, and Garbe P. The economic burden of asthma in the United States, 2008-2013. Ann Am Thorac Soc. 2018;15(3):348-56.
Patel SJ, Bergert L, Longhurst CA, Sharek PJ. The Joint Commission’s asthma care measure set: How does it measure up? Agency for Healthcare Research and Quality. 2013. saludequitativa.blogspot.com/2013/05/national-quality-measures-clearinghouse.html?m=1
Pyle RC, Divekar R, May SM, et al. Asthma-associated comorbidities in children with and without secondhand smoke exposure. Ann Allergy Asthma Immunol. 2015;115(3):205-10.
Sapir T, Moreo KF, Greene LS, et al. Assessing patient and provider perceptions of factors associated with patient engagement in asthma care. Ann Am Thorac Soc. 2017;14(5):659-66.
Zipkin R, Schrager SM, Nguyen E, Mamey MR, Banuelos I, Wu S. Association between pediatric home management plan of care compliance and asthma readmission. J Asthma. 2017;54(7);761-7.


















