Remove the trauma of healthcare visits for this patient population.
- Patients with deafblindness have needs beyond the basic knowledge provided in most nursing schools regarding hearing and visual impairment.
- Although 45,000 to 50,000 Americans experience the effects of deafblindness, only 1% have both total blindness and hearing loss; 5% are totally blind, and 20% have profound hearing loss.
- These patients require specialized and personalized services that are more complex than those designed solely for deaf or blind people.
Patients with moderate-to-severe visual and hearing impairments (deafblindness) need their nurses to understand their needs and provide safe care. Nurses have fundamental knowledge about caring for patients with glasses, placing food positionally for a blind patient, ensuring a patient with hearing loss has their hearing aids, and speaking clearly when a patient has difficulty understanding. Patients with deafblindness, however, have needs beyond the basic knowledge provided in most nursing schools.
Skilton and colleagues describe those with deafblindness as a “hard-to-reach” audience faced with communication barriers, limited budgets, lack of training in healthcare accessibility, and sensory impairment self-awareness. However, with the right preparation, nurses can appropriately assess pain, implement de-escalation techniques, and advocate for their patients.
Deafblindness defined
A person with deafblindness experiences a degree of both vision and hearing loss. Many believe that individuals with deafblindness experience total vision loss and total or profound hearing loss. However, according to Vanderbilt University, although 45,000 to 50,000 Americans experience the effects of deafblindness, only 1% have both total blindness and hearing loss; 5% are totally blind, and 20% have profound hearing loss.
About 70 conditions and disorders cause deafblindness, including premature childbirth and intrauterine prenatal complications such as cytomegalovirus, microcephaly, and hydrocephaly. Patients diagnosed with CHARGE (coloboma, heart defects, atresia choanae, growth retardation, genital anomalies, and ear abnormalities) syndrome, Down Syndrome (Trisomy 21 Syndrome), and Usher Syndrome (genetic disease affecting vision and hearing) may exhibit deafblindness. Others may develop deafblindness as a result of asphyxia, meningitis, severe head injuries, or unknown causes. As a result of expected delays in language and milestone development, these patients may receive diagnoses of mild, moderate, or severe intellectual disabilities and cognitive impairments. Depending on cognitive ability and language development before acquiring deafblindness, people with this condition can communicate fluently. However, fluency also is influenced by socioeconomic status, accessibility to assistive technology, socialization, and intellectual abilities. Early detection and intervention can help members of this population experience the best quality of life.
Prepare for the patient
Medical appointments and healthcare encounters can be confusing for many people with deafblindness. They require specialized and personalized services that are more complex than those designed solely for deaf or blind people. In addition, most, if not all, have difficulty with communication, orientation and mobility (O&M), and access to information. Difficulty accessing information is secondary to the individual’s physical state and their delay in processing information (cognitive impairments).
Many people with deafblindness have behavioral challenges, such as difficulty with impulse control, anxiety, attention to a task, and risk for elopement. You may see these behaviors escalate during a medical visit or procedure depending on the patient’s cognitive function and comfort level with medical professionals. To prepare yourself, the setting, and the patient, implement strategies for a successful encounter, including incorporating effective and personalized communication techniques, establishing a safe environment, and preventing behavioral escalation.
Establish communication techniques
Communication methods may differ depending on whether the patient acquired deafblindness congenitally or later in life. If the latter, their exposure to language in early childhood may provide them with a broader knowledge of communication. Other factors to consider when selecting communication methods include the patient’s literacy level and degree of visual and auditory deficit. If possible, enlist a speech therapist to help with communication evaluation and techniques.
Older patients may have assistive devices for communication or established techniques. Some patients with deafblindness use a combination of communication methods depending on the recipient and the situation. You’ll want to customize the communication techniques to the individual patient and their family based on the patient’s language development and physical and cognitive abilities.
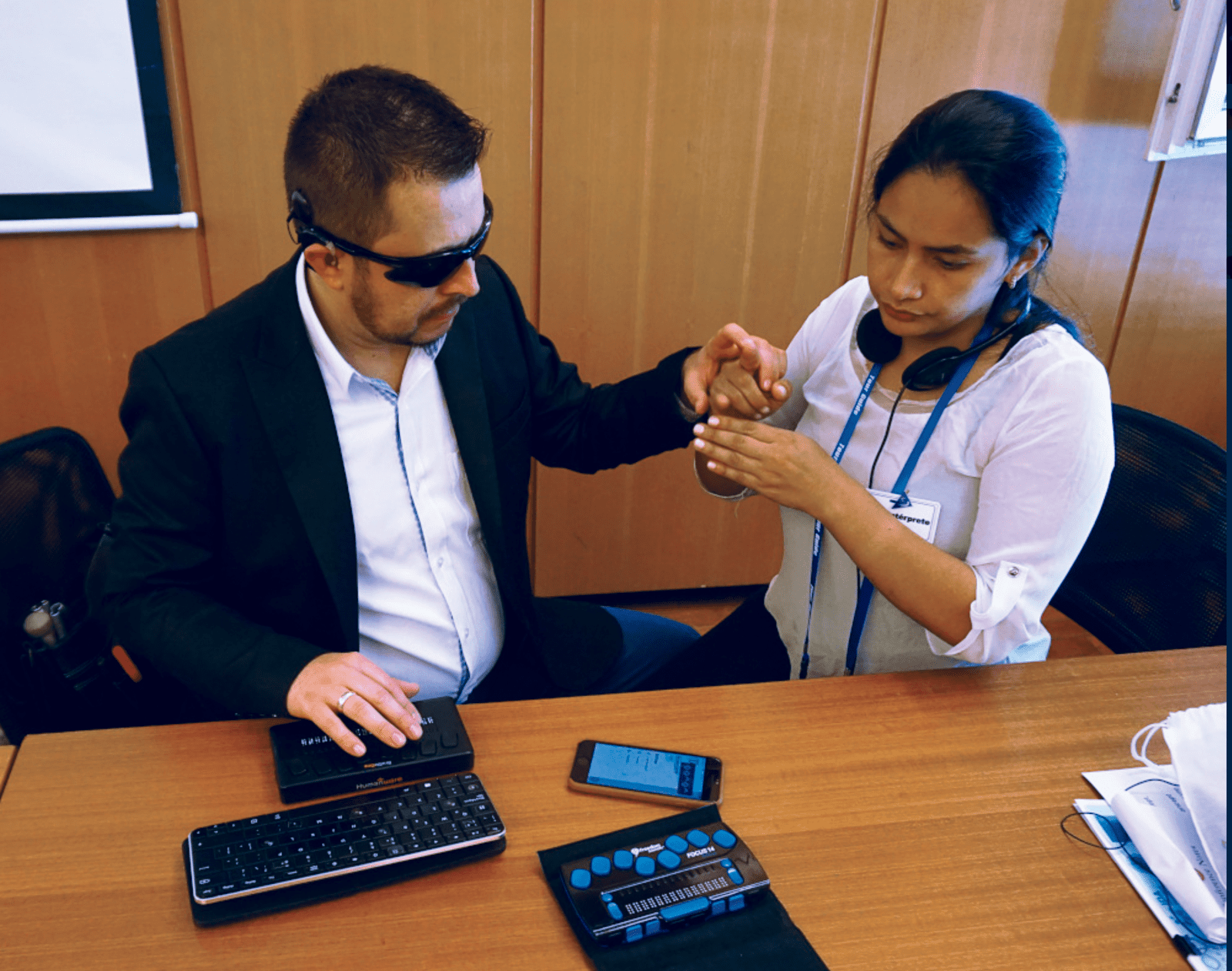
Begin an outpatient meeting by explaining the reason for the visit and describing the assessments and procedures you’ll perform. Before you begin your assessment or intervention, allow the patient to explore the healthcare area. Let them touch the equipment, guiding their hands and the equipment to the associated body part. To help prevent behavioral escalation, give them at least 5 seconds to process the information about each element. In an emergency or acute care situation, you may not be able to prepare the patient, so communicate assessments and procedures in real time with the patient or family while optimizing time for processing as much as possible. (See Communication methods.)

Communication methods
Patients with deafblindness may use the following communication methods to express and receive language.
- Behavior/routines
- Body language
- Braille
- Co-active signing
- Communication devices
- Deafblind manual alphabet
- Facial expressions
- Gestures
- Key word sign (formerly known as Makaton)
- Lip reading
- Object symbols
- Pictures/photos
- Print on palm
- Speech
- Signed English
- Sign language with unique distinctions from individual countries (American, British, French, Japanese, Vietnamese, etc.)
- Signs used on the body
- Social haptics
- Tactile signing
- Tracking
- Visual frame signing
- Written (large print written or typed information)
To learn more about these methods, visit deafblindinformation.org.au/living-with-deafblindness/deafblind-communication.
Create a safe environment
Maintaining safety protects the patient and others in the room. Ensure the patient can move freely around medical personnel and equipment, and remove any harmful or sharp objects in case behavioral escalation occurs. Before touching the patient, warm your hands and instruments. If the patient uses a hearing device (hearing aid, cochlear implant, amplifying system), ensure it’s working properly. The environment shouldn’t be too loud; avoid startling sounds. In emergency and acute situations, quickly perform surveillance of the environment for objects obstructing mobility and anything that might cause harm.
If your organization has an O&M specialist, use their expertise to prepare for the patient. O&M specialists assist with evaluations and provide guidance to help patients with visual impairments maneuver as independently as possible throughout their home, work, and community environments. The specialist can help rearrange the room and assist the patient to move around the unfamiliar environment using their assistive devices. Proper orientation increases patient confidence and decreases anxiety and escalation. If you’re working without O&M specialists, concentrate on safety (perform a patient-focused assessment, and implement fall prevention and patient education techniques) while ensuring adequate communication, proper guidance, and environmental orientation.
Prevent behavior escalations
According to the National Center on Deaf-Blindness, 87% of children and youth on the National Deaf-Blind Child Count have additional disabilities. In 2021, 76% had speech and language impairments and 64% experienced cognitive impairments. Many children also have complex medical needs and behavioral challenges.
To prepare for an outpatient visit, the office should contact the family to establish a social story (a tool used by parents, patients, and professionals to explain and establish expectations for anticipated interactions). A family member or healthcare staff can review the social story with the patient to help lower anxiety and reduce risk of behavioral challenges during the visit. You may witness tantrums, loud vocalizations, throwing objects, or self-injurious behaviors such as head banging, biting, hitting, or scratching. Be prepared to recognize signs of anxiety and intervene before behavior escalates.
To help reduce the risk of irritability, Belote suggests speaking with the family before the visit to ensure the patient has eaten and toileted. Also ask about preferred items you should have available to aid patient comfort. Many clinical settings use certified child-life specialists (from birth up to age 21) to prepare healthcare environments. These experts create therapeutic plans using developmental and psychological activities and interventions to improve patients’ and families’ healthcare experience. They may provide activities and use techniques to establish a calm environment and meet the patient’s developmental needs. For adults, a social worker can provide similar assistance.
In emergency and acute care settings, social workers can offer resources to patients, families, and staff to improve healthcare encounters. Acute care and emergency settings should be made aware of the patient’s level of sensitivity to avoid unscheduled disruptions.
Patient advocacy during care delivery
Use “checkpoints” throughout the healthcare encounter to assess the patient’s comfort level and understanding. People who are deafblind frequently vocalize excitement, anger, discomfort, and anxiety, or when requesting an item or activity. If the patient has a family member or community advocate with them, clarify the meaning of the different vocalizations. Ensure that assessments, interventions, and outcomes include consideration for your patient’s deafblindness when developing nursing care plans, and allow patients to participate to the extent of their ability.
Research state and national deafblind outreach projects, including the Helen Keller National Center for Deaf-Blind Youth and Adults, the American Association of the Deaf-Blind, and the National Family Association for Deaf-Blind. Most outreach projects offer early intervention for children during primary development, including technical assistance to patients, families, and educational teams. Specialists can help with interprofessional care across the lifespan. Certified child life specialists, social workers, orientation and mobility specialists, speech therapists, and nurses should work together with patients to ensure they receive holistic care that improves the healthcare experience and their quality of life.
De-escalation tactics and trust
If a behavioral escalation occurs, make sure the environment is safe (remove objects that can be thrown) and seek additional support from colleagues if warranted. Position yourself between the patient and the door; remain calm and don’t touch the patient without first communicating your intent and obtaining their understanding. Unwarranted physical touch can exacerbate anxiety, frustration, or anger. After the patient calms down, lightly tap their shoulder to indicate your need for their attention and to notify them that communication will occur.
Patients with aggressive behavior and those diagnosed with moderate-to-severe intellectual disability, significantly contribute to the frequency of employee injury. Use behavioral protective equipment, such as arm sleeves, to block bites and scratches, shin guards to protect lower limbs, and a body guard to protect the trunk. Some patients with deafblindness may injure themselves by hitting or banging their heads on walls and objects. A study by Romani and colleagues found that using blocking and other preventive measures, rather than restraints or seclusion, can help reduce staff injuries.
Pain expression and assessment
 Pain assessment tools vary in levels of effectiveness in patients with deafblindness. For example, a visual pain scale isn’t appropriate for a patient with a high degree of visual impairment, and verbally asking a patient to rate their pain on a scale from 1 to 10 isn’t effective for those with severe auditory deficits. Patients with deafblindness may be able to show you a picture or use their augmentative and alternative communication device to communicate the presence of pain. They also may use sign language, vocalize, or draw your attention to the painful area by guiding your hands to it.
Pain assessment tools vary in levels of effectiveness in patients with deafblindness. For example, a visual pain scale isn’t appropriate for a patient with a high degree of visual impairment, and verbally asking a patient to rate their pain on a scale from 1 to 10 isn’t effective for those with severe auditory deficits. Patients with deafblindness may be able to show you a picture or use their augmentative and alternative communication device to communicate the presence of pain. They also may use sign language, vocalize, or draw your attention to the painful area by guiding your hands to it.
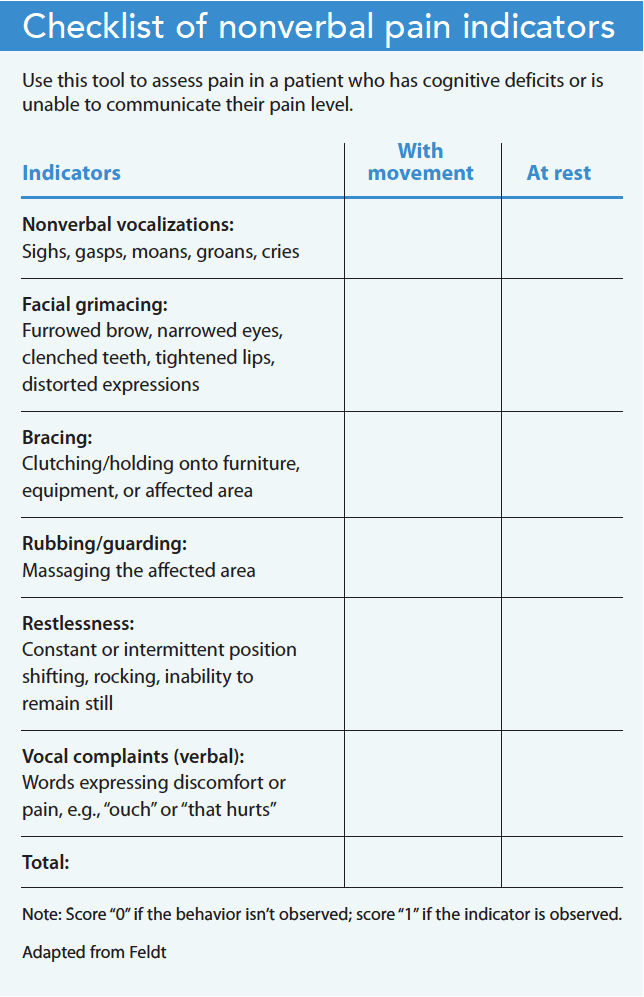
Some individuals with deafblindness communicate through behavior. The Checklist of Nonverbal Pain Indicators (CNPI), developed to address the lack of assessment tools available to determine pain in cognitively delayed patients (particularly older adults), can prove useful when assessing pain in this patient population. Feldt noted that using the CNPI provided comparable results for cognitively intact and impaired patients. In this 1995 study, 35 cognitively intact and 53 cognitively impaired patients participated. Feldt reported that the most common behavior at rest was facial grimacing, which was observed in 30.6% of the impaired patients and 20.6% of intact patients. The second most frequent behavior observed in impaired patients at rest was restlessness (20.4%). (See Checklist of nonverbal pain indicators.)
Feldt also noted that cognitively intact patients received more pain medication than cognitively impaired patients. Observe and assess pain in patients with deafblindness using nonverbal and behavioral cues, and advocate on their behalf by notifying the provider of the need for pain management.
Make a positive impact
Without appropriate communication, environmental safety, and behavioral de-escalation assistance, healthcare encounters can cause traumatic experiences for this patient population. Debrief with the patient, family, and colleagues about how to improve future visits, and include that information in the patient’s electronic health record. Remember to celebrate successful encounters by giving the patient positive feedback or a thumbs up if you’re unfamiliar with sign language. A smile goes a long way.
Preshus Brooks is the nursing supervisor for residential services at Children’s Home Association of Illinois in Peoria. She previously served as nurse manager at Philip J Rock Center & School in Glen Ellyn, Illinois.
American Nurse Journal. 2023; 18(9). Doi: 10.51256/ANJ092323
References
Belote M. Fact sheet: Strategies for successful medical/dental appointments for individuals who are deaf-blind. California Deaf-Blind Services. 2006. sfsu.edu/~cadbs/20MedicalAppts.pdf
Deafblind Information Australia. Living with deafblindness: Deafblind communication. deafblindinformation.org.au/living-with-deafblindness/deafblind-communication
Feldt KS. The checklist of nonverbal pain indicators (CNPI). Pain Manag Nurs. 2000;1(1):13-21. doi:10.1053/jpmn.2000.5831
National Center on Deaf-Blindness. 2021 National Deaf-Blind Child Count Report. 2022. nationaldb.org/products/national-child-count/report-2021
Romani PW, Ariefdjohan M, Jensen Gaffey LL, Torres‐Dominguez M, Lister J. Relations between patient and staff member characteristics and staff member injury on a psychiatric inpatient unit for children with intellectual or developmental disabilities. J Child Adolesc Psychiatr Nurs. 2020;33(3):125-30. doi:10.1111/jcap.12291
Skilton A, Boswell E, Prince K, Francome-Wood P, Moosajee M. Overcoming barriers to the involvement of deafblind people in conversations about research: Recommendations from individuals with Usher syndrome. Res Involv Engagem. 2018;4:40. doi:10.1186/s40900-018-0124-0
Vanderbilt University. Introduction to language and communication: Deaf-blindness. my.vanderbilt.edu/speds2430/2020-topics/deaf-blindness
Key words: deafblindness, healthcare trauma, health advocacy