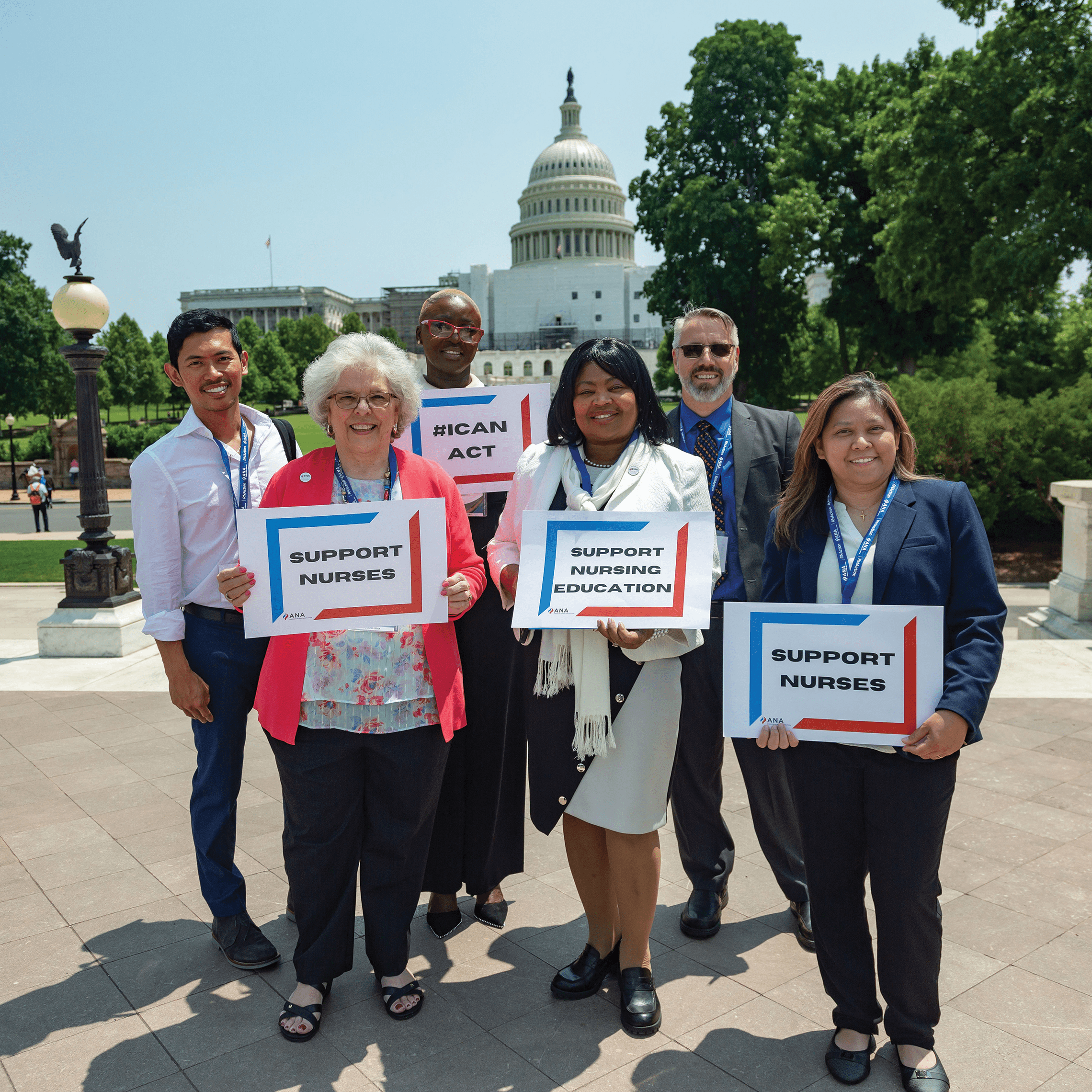
2024 priorities include nursing workforce protections, access to nursing care, and payment parity.
The end of the first session of the 118th Congress was notable, to say the least. For starters Speaker of the House Kevin McCarthy (R-CA) was removed and a relatively unknown lawmaker, Mike Johnson (R-LA), was elected to the role following a tumultuous 3 weeks of nominations, votes for, and withdrawals of other candidates. Subsequently, the spending budget that passed the House of Representatives was lower than the number that had been agreed to by the President of the United States and House Republicans just a month before in the debt ceiling negotiations.
This is new territory for the American Nurses Association (ANA) and other organizations that advocate for healthcare and healthcare professionals.
As Congress settles into 2024 and a presidential election year, ANA is pursuing nursing priorities by advocating across a broad range of issues important to nurses and the profession. The association continues to engage with the Biden-Harris administration and key federal agencies on nursing priorities, including promoting and protecting the nursing workforce, removing practice barriers for advanced practice RNs (APRNs), and achieving payment parity for nurses.
The elevator pitch: A 60-second advocacy tool for nurses
Speak to be heard: Effective nurse advocacy
Here’s a look at progress made in 2023 and priorities for 2024.
Nursing education
One of the biggest bottlenecks to getting more people trained and educated as nurses is the longstanding faculty shortage in our country. This crucial gap is due largely to low starting salaries for faculty positions and high student loan amounts owed by recent graduates. ANA proudly participated in creating the Nurse Faculty Shortage Reduction Act (S. 2815), which Sens. Richard Durbin (D-IL) and Lisa Murkowski (R-AK) introduced in the Senate in July. This bipartisan bill would create a 5-year pilot project for schools of nursing to apply for grants from the Health Resources & Services Administration to supplement the difference between what faculty nurses are paid versus what equally trained critical care nurses earn.
ANA also proudly supported introduction of the Educating Future Nurses Act (S. 1586/H.R. 3623). This bill would establish a permanent funding stream in Medicare for hospitals to partner with schools of nursing, community-based care settings, and other hospitals to increase clinical education for APRN students. The idea for the bill came from a similar 5-year pilot program included in the Affordable Care Act. The latter proved to be highly successful, according to an analysis published in Health Affairs. The bill is also part of the Site-based Invoicing and Transparency Enhancement (SITE) Act (S. 1869).
Nurse staffing
The 2022 ANA Membership Assembly—the association’s governing and official voting body—approved a recommendation to include staffing ratios as an option for relieving the longstanding staffing issues, including nurse burnout, brought to light by the COVID-19 pandemic. After extensive conversations with several stakeholders, the ANA Board of Directors voted to endorse the Nurse Staffing Standards for Hospital Patient Safety and Quality Care Act
(S. 1113/H.R. 2530). This federal bill would establish minimum nurse-to-patient ratios for every hospital. ANA supports nurse staffing ratios as part of a larger solution to solve the current crisis. In addition to establishing minimum nurse-to-patient staffing requirements at the national level, S. 1113/H.R. 2530 would help examine best practices for nurse staffing and provide whistleblower protections for nurses who choose to advocate for the safety of their patients.
State laws have been enacted to address nurse staffing levels, but they require adequate enforcement to promote nurse retention, help alleviate nurse burnout, and address other challenges that nurses face daily. In addition to staffing levels, key work environment issues include workplace violence, mandatory overtime, and reimbursement/compensation. These issues have caused widespread and historic nurse strikes.
Long-term care minimum staffing rule
In 2023, ANA maintained pressure on the Department of Health and Human Services (HHS) and its subagency the Centers for Medi-care and Medicaid Services (CMS) to address the nurse staffing crisis. ANA has called for HHS to convene a diverse set of stakeholders in a conversation to identify short- and long-term solutions to nurse staffing challenges. This includes CMS using all available current regulations and enforcement mechanisms to ensure a safe environment for nurses while the agency completes rulemaking started in September 2023.
CMS issued a proposed rule in September setting minimum nurse-to-patient ratios in long-term care facilities. ANA submitted comments mostly supporting the rule and asking for certain changes in the final rule. We celebrated the rule’s inclusion of a 24/7 RN requirement for these facilities—a policy the association has long advocated for. However, the comment noted that the rule didn’t include LPNs in its ratio calculation and provided unclear enforcement mechanisms. In 2024, ANA looks forward to CMS quickly issuing a final rule that incorporates this feedback and ensures that nurses are primary stakeholders when meeting with HHS.
Workplace violence
Workplace violence continues to serve as a major driver of burnout among and a serious cause of harm to nurses. Tragically, in October 2023, a nurse doing a home visit was murdered in Connecticut. Congressional and agency action must occur to ensure nurses have safe and healthy work environments. ANA believes Congress must act to protect nurses and acknowledge the key role employers play in minimizing the risk of violence on-site. The association continues to advocate for passage of the Workplace Violence Prevention for Health Care and Social Service Workers Act (S. 1176/H.R. 2663). This crucial legislation would require the Occupational Safety and Health Administration (OSHA) to develop and enforce specific standards for healthcare and social service employers, which would hold employers accountable for protecting their staff from workplace violence. The House has passed this legislation twice—in the 117th Congress, with significant bipartisan support, and in the 116th Congress—but the Senate so far has failed to act.
ANA has long advocated for OSHA to issue a standard focused on preventing workplace violence in healthcare settings. In May 2023, OSHA began its official rulemaking process with a required review of a draft standard. This review convened panels of small business owners in the healthcare and social assistance fields who gave initial feedback on the draft standard. ANA submitted comments on this draft and review process and urged OSHA to quickly continue this rulemaking. The draft standard implements OSHA’s guidelines from 2016, which help employers create tailored prevention programs depending on their unique setting and risk factors.
In addition, ANA has endorsed the Senate version of the Safety from Violence for Healthcare Employees (SAVE) Act (S. 2768). This bill would create federal legal penalties for individuals who knowingly and intentionally assault or intimidate hospital employees. ANA is endorsing only the Senate version, and not the House version, because the Senate’s version includes a study on the judicial process and prosecutions to see if making assault against healthcare workers a federal crime has improved the rate of prosecution or diminished it even further.
Improving patient access to quality APRN care
APRNs frequently provide primary and maternal healthcare in areas with limited access to physicians, such as medically underserved urban and rural areas. More than 83% of nurse practitioners treat Medicare patients and the profession is now the highest biller of Medicare, outpacing physicians. A compelling need exists to reform Medicare laws to accommodate common healthcare practices and eliminate outdated arbitrary barriers, which were created before APRNs could even participate in the Medicare program. This is why ANA is advocating for passage of the Improving Care and Access to Nurses (ICAN) Act (S. 2418/H.R. 2713). The bill would permanently remove barriers to care and increase access to high-quality services provided by APRNs under Medicare.
APRNs are highly qualified clinicians in their specialty fields. Yet many outdated Medicare regulations continue to restrict APRNs from caring for their patients without physician supervision or receiving payment for certain services. ANA contends that APRNs must be allowed full practice authority in federal programs aligned with their state licensure. In 2023, we saw movement toward this goal as CMS started using the term “practitioner” whenever possible in regulations and guidance instead of specifying “physician.” This shows CMS is changing to a structure that values and includes APRNs. CMS also implemented pieces of the Balanced Budget Act of 2018 in which Congress required CMS to allow APRNs to supervise cardiac and pulmonary rehabilitation services.
In 2024, ANA will continue to advocate for CMS to release the final Provider Nondiscrimination Rule, which would prevent discrimination in payment, contracting, and unnecessary practice restrictions, and allow APRNs to practice to the top of their license in federal health programs.
Payment parity and transparency
It’s beyond time for nursing care to be truly valued and paid transparently. However, federal payment systems hide the impact of RNs behind physician expenses or other service charges. In 2023, ANA launched the National Provider Identifier (NPI) campaign. By registering for an NPI, nurses can urge systems to extract nursing services from their data and demonstrate the critical role of nurses in patient care. ANA also encourages all APRNs to apply for an individual NPI. Many APRNs bill through their employer. Obtaining an individual NPI doesn’t keep APRNs from continuing to bill through their employer. Rather, having an individual NPI positions an APRN to open their own practice, as Medicare, Medicaid, and most private payers require an NPI for reimbursement.
In 2024, ANA will continue to push CMS and all health systems to move toward nurse pay transparency and parity through direct advocacy and our NPI campaign. Register for an NPI today at nursingworld.org/npi.
As the year unfolds, ANA will remain alert and agile in advocating on behalf of America’s over 5 million RNs. All nurses can bolster these advocacy efforts by engaging in grassroots advocacy opportunities. Individual nurse participation, whether through their state associations or directly with ANA at the federal level, adds up and can lead to significant legislative and policy wins.
Stay up to date and engage with policy advocacy in the following ways:
- Sign up for Action Alerts in the Action Center at rnaction.org. Action Alerts inform participants when we need them to email their policymakers. This simple and easy step takes just moments but can make a significant difference when all participants make their voices heard.
- Read the Capitol Beat Blog at anacapitolbeat.org. This platform dives into policy issues and keeps the national nursing community apprised of actions in Congress and by the administration that affect nurses, the nursing community, and their patients.
- Follow ANA social media channels. @RNAction posts the latest news about issues impacting nursing on Facebook and X (formerly Twitter).
ANA is proud to work alongside its members, constituent and state nurses associations, and individual nurses across the country to ensure that decision-makers in Washington, DC, hear what nurses need most.
— Sam Hewitt is principal for federal affairs and Emily Champlin is senior policy advisor at ANA.
American Nurse Journal. 2024; 19(3). Doi: 10.51256/ANJ032432