Evidence-based recommendations.
Takeaways:
- Inadequate postoperative pain relief can increase length of stay, delay discharge, increase readmission rates, and delay ambulation.
- Exploring the postoperative challenges faced by patients with chronic pain can help nurses identify and implement safe and effective multimodal palliation strategies.
- Nurses are uniquely positioned to act as liaisons between patients and an interdisciplinary care team to mitigate postoperative pain.
Learning Objectives:
- Describe preoperative pain assessment and education.
- Discuss the pharmacologic management of pain in postoperative patients.
- Identify patients at risk for adverse effects of postoperative pharmacologic pain management.
The authors and planners of this CNE activity have disclosed no relevant financial relationships with any commercial companies pertaining to this activity. See the last page of the article to learn how to earn CNE credit.
Expiration: 12/1/24
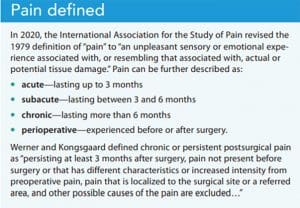
Patients with chronic pain are at higher risk for uncontrolled pain during and after surgery. Nurses can serve as liaisons between patients and an interdisciplinary team to mitigate pain. To be effective in this role, nurses need to understand recommendations for preparing patients with chronic pain for surgery, how to set expectations for pain management, and pharmacologic and nonpharmacologic treatment options. (See Pain defined.)
Perioperative pain
Pain is the biggest concern expressed by perioperative patients. According to the 2011 U.S. Institute of Medicine report Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research, 80% of patients who underwent a surgical procedure reported postoperative pain. Of those patients, 88% reported moderate, severe, or extreme pain. Adequate postoperative pain control is essential to ensure optimal physical functioning and mental health, sustain relationships, and help patients return to work or regular activity. Poorly managed pain can increase hospital length of stay, increase readmission rates, and decrease patient satisfaction. Despite improved understanding of pain mechanisms, enhanced awareness of the prevalence of postsurgical pain, and improved pain-management approaches, inadequately controlled postoperative pain remains a widespread problem.
In 2016, the American Society for Regional Anesthesia (ASRA) guideline panel concluded that optimal postoperative pain management begins preoperatively. It’s achieved via detailed assessment and a care plan tailored to the patient and surgical procedure, with follow-up assessments and modifications as needed. Nurses are critical to this process because of the amount of time they spend with patients. Enhanced recovery after surgery (ERAS) protocols detail the benefit of patient preparation for surgery using evidence-based approaches to achieve functional outcomes. Engaging patients in pain management through preoperative educational programs that create a partnership can lead to greater patient satisfaction and action-orientated goals such as DREAMS (drinking, eating, analgesia, mobilizing, and sleeping; cheers-dream.com).
Nurses’ role in pain management
The nurse’s role in caring for patients with acute surgical pain is particularly critical when those patients have preexisting chronic pain. In collaboration with an interdisciplinary care team, you can develop and administer care plans that promote comfort, facilitate recovery, and restore physical, emotional, and social health. The nursing process can support this practice via enhanced pain assessment, nursing diagnoses, care planning, and implementation and evaluation of perioperative interventions that support this vulnerable population.
Cultivate your pain assessment and re-assessment skills through mentoring, experience, and adherence to an organizational policy that values patient feedback and continuous quality improvement. Collect, review, and analyze data recorded in the electronic health record and ancillary staff reports (for example, vital signs and patient self-report of pain intensity score and comfort). Review medication effects, the impact of pain on functional gains, and adverse side effects of medication or other treatment strategies. Then systematically and critically examine this dynamic patient data and incorporate iatrogenic risk, sedation level, and respiratory and functional status to establish a nursing care plan. The entire process should be informed by patient self-report and your clinical assessment. As a patient advocate, you can contribute to the care team’s development of a multimodal treatment plan.
Preoperative actions
Before surgery, to better understand the patient’s current experience with pain, take a pain history, perform medication reconciliation, assess the patient’s baseline pain, and provide patient education. (See Preoperative challenges.)
Pain history and medication reconciliation
To help develop a comprehensive postoperative pain plan, collaborate with patients to obtain a thorough history. Clarify current areas of discomfort and ask about previous effective and noneffective medications. Conduct a comprehensive review of prescribed and nonprescribed home medications, including opioids, nonopioid adjuvants, over-the-counter pain relief agents, herbal supplements, and medication-assisted treatment (MAT) for opioid use disorder.
Patients who are already prescribed opioid medication as part of their home regimen may require higher opioid doses to adequately manage acute surgical pain. During the postoperative period, vigilantly assess these patients for opioid-induced respiratory depression and cognitive effects, including confusion or lethargy.
Failing to maintain a patient’s opioid, benzodiazepine, and other adjuvant home regimens may put them at risk for withdrawal or undertreatment. Opioid withdrawal isn’t lethal, but it can influence acute pain assessment, limit mobility, and slow functional progress, resulting in unnecessary pain. Benzodiazepine and alcohol withdrawal can be fatal and requires comprehensive assessment.
Universal screening helps normalize conversations about substance use and decrease the associated stigma. Use valid and reliable screening tools to identify this population, which includes patients who currently use alcohol or illegal substances to palliate chronic pain. Show empathy and focus on ensuring safety and adequate pain control.
Baseline pain assessment
Make baseline pain assessment a preoperative priority and perform a comprehensive biopsychosocial assessment on admission to help guide the nursing care plan. Document information and share it with the care team to ensure that chronic pain symptoms aren’t mistaken for an acute pathology and that new, potentially dangerous symptoms aren’t disregarded as a chronic condition. For example, consider a patient’s previous deficits in sensation, range of motion, physical functioning, and tolerance, which may contribute to the current pain assessment.
Your baseline pain assessment should include specific pain locations, pain quality and character, onset, duration (minutes, hours, months, years), frequency or consistency, and severity. To determine pain severity, ask questions related to patient-identified goals. For example, ask if they’re comfortable enough to walk in the hallway or eat breakfast. Base subsequent focused pain evaluations on this initial comprehensive assessment. Significant changes should trigger a more detailed evaluation and care team collaboration.
Preoperative education
A well-designed preoperative educational program includes understanding the patient’s pain experience, expectations, and previous use of multimodal strategies. Include the patient and their chosen support team in the care planning process, and provide education before the surgery date to help ensure expectations are congruent with safe practice.
Patients with chronic pain may have had previous healthcare experiences in which their pain wasn’t well controlled. These experiences may lead to fear avoidance, anxiety, depression, or catastrophizing. Collaborate with patients to understand their past experiences, and guide the education to relieve these concerns.
Discuss multimodal pain management strategies, including nonpharmacologic, nonopioid, and opioid options, as well as opioid limitations. Also include nonpharmacologic self-care and self-management interventions to enhance the postoperative pain treatment plan.
Postoperative management
Postoperative pain management for patients with chronic pain includes pain assessment, nonpharmacologic and pharmacologic interventions, and discharge education.
Pain assessment
Managing acute postoperative pain relies on accurate assessment. The perpetual pain assessment and re-assessment cycle creates a symbiotic relationship between the patient and the nurse, establishing the foundation for developing a comprehensive pain management regimen that addresses the physical, emotional, and spiritual domains of the pain experience. Pain is a personal, unique, and subjective experience that can be challenging to assess and manage. This challenge is amplified when patients have a chronic pain condition.
Compare postoperative assessments with the preoperative and chronic pain baseline assessments, including physiological, psychological, sociocultural, spiritual, economic, and lifestyle factors. Also include the physical causes and manifestations of pain and the patient’s response to interventions. This biopsychosocial approach provides the foundation for interdisciplinary pain care.
Pain measurement vs. assessment
The complex symptom of pain requires refined measurement and assessment skills. Pain measurement refers to patients assigning a number to their pain level, most commonly on a 0 to 10 scale. Pain assessment refers to obtaining subjective and objective data. Numerical pain scores comprise a component of the overall pain assessment but shouldn’t serve as a stand-alone value to determine a treatment plan. An American Society for Pain Management Nursing position statement elaborates on the consequences of this practice and the risk of opioid overdose. Dosing and administering medications, such as opioids, based solely on a numeric pain score undermines your assessment and leads to rote administration of medication without critical thinking and patient collaboration.
Determining the cause of pain in a surgical patient may appear straightforward, but can pose challenges when caring for a patient with a history of chronic pain. Differentiating a new potential source of pain related to surgery from other possible causes requires polished assessment skills. With the advent of contemporary regional anesthesia techniques, the source of pain may not be the surgical site. Instead, the source could be a chronic pain condition, positioning, or a new and undiagnosed condition such as deep vein thrombosis or pressure injury from immobility.
Never assume the location of a patient’s pain. Talk with them about what they’re feeling and how it relates to their chronic pain. If a patient reports a painful sensation, visually assess and inspect the location. When possible, gently palpate the pain area to determine if the skin is intact and to evaluate for any neurologic or musculoskeletal deficits.
The ASRA panel recommends a multimodal pain management regimen tailored to the patient, setting, and surgical procedure. Acute surgical pain requires a multifaceted approach that includes medication, nerve blocks, physical therapy, and other modalities. When clinically indicated, consider an integrative and collaborative approach to postoperative pain management. Nursing care plans should take into account the patient’s physical condition, including any incisions, wounds, drains, or equipment that may amplify pain, impair comfort, and impede function.
Based on your assessment, create an integrated plan that includes nonpharmacologic and pharmacologic options.
Nonpharmacologic interventions
The Joint Commission’s 2018 pain standards support the use of nonpharmacologic postoperative interventions, many of which are within the scope of nursing practice and don’t require a provider order to implement. Work directly with patients to identify nurse-driven nonpharmacologic pain management modalities, such as music, guided imagery, reiki, aromatherapy, acupuncture, reflexology, and other mind–body approaches that can help downregulate the sympathetic response to stress. Just as stress and anxiety can amplify pain perception, these interventions can provide a sense of calm and control, leading to a perception of less pain without additional medication. Avoid any misleading descriptions of these interventions that imply they can diagnose, treat, or cure a condition.
Regardless of the intervention chosen, patient engagement is essential. Underscore that nonpharmacologic interventions aim to enhance comfort and self-determination, not to withhold pain relief.
Some modalities require planning, so educating patients about them before surgery may decrease barriers to access. Regardless of the interventions selected, provide instruction and allow repetition and practice to enhance patient confidence and increase use. (See Nonpharmacologic intervention options.)

Pharmacologic management
Opioids provide a fundamental aspect of acute, postoperative pain management, but not without risk. Common opioid-related adverse drug events after surgery include nausea, vomiting, constipation, pruritus, sedation, and respiratory depression. Urman and colleagues note that such occurrences have been reported in 9.1% to 11.5% of adults. Accordingly, evidence-based practice recommendations support a multimodal pharmacologic approach, including preventive analgesia, nonopioid medications, and regional anesthesia techniques, such as continuous catheter-based local anesthetic infusion.
The consistent use of nonopioid medications may reduce opioid requirements and enhance function. Advocate for around-the-clock nonopioid complements, such as acetaminophen and nonsteroidal anti-inflammatory medications, when prescribed. Patients may hesitate to accept these medications, perceiving them as a replacement for an opioid that may not adequately control pain. Emphasize that nonopioid complements serve to enhance comfort. Explain the stepwise approach, in which nonpharmacologic interventions and nonopioid adjuvants can decrease opioid use. However, if patients don’t achieve adequate palliation of pain intensity using these interventions, promptly administer the prescribed as-needed opioid medication barring sedation or other safety concerns. Never withhold opioids solely to demonstrate diminished opiate consumption. This may result in patients feeling marginalized and distrustful of the healthcare system.
At-risk patients
Some patients may be at risk for iatrogenic opioid addiction, whereas others may have a pre-existing substance use disorder (SUD) or opioid tolerance or dependence. In addition, some patients may be prescribed MAT for SUD. All of these patients require close assessment and monitoring and careful management to avoid negative outcomes while still ensuring adequate pain control.
Iatrogenic addiction. Patients may be at risk of becoming new chronic opioid users in the postsurgical setting if care isn’t taken to mitigate risk. Patients at risk for chronic opioid use include those with a family history of addiction, or a personal history of tobacco use, SUD, anxiety, depression, and other pain disorders. This information, identified during the initial preoperative assessment, can facilitate risk reduction strategies, including preemptive specialist pain management or behavioral healthcare for treatment optimization and perioperative recommendations. Speak with providers about incorporating opioid-sparing interventions such as local anesthetic infiltration, nerve blocks, and regional anesthesia to enhance the multimodal analgesia plan.
SUD. Organizations should consider universal screening for SUD. This may include using an opioid risk tool (such as Screening, Brief Intervention and Referral to Treatment, or the Opioid Risk Tool) and reviewing the state prescription database for all patients. The perioperative team may consider urine drug toxicology screening for patients deemed high-risk. For patients who have a pre-existing SUD, consult with an addiction medicine or acute pain specialist to ensure they receive safe and effective pain care. Uncontrolled pain in these patients may increase the likelihood of risky postoperative behavior to pursue pain relief. Patients with alcohol use disorder may prompt the perioperative team to reconsider the timing of elective surgery to allow for safe alcohol detoxification.
Explain to patients that the steps you’re taking are guided by pain palliation and safety goals.
Opioid tolerance and dependence. Patients prescribed opioids can develop tolerance and physical dependence. Opioid tolerance is defined as a reduction in the effect of an opioid after prolonged administration. The evolution of an individual’s tolerance depends on the medication’s interactions with the opioid receptors, the dose, and administration frequency. Contributing mechanisms include upregulation (increase in the number of receptors, which occurs when receptor activity is lower than usual) or downregulation (decrease in the number of receptors, which occurs when receptor activity is higher than usual) of drug metabolism, desensitization of receptor signaling, and the initiation of compensatory–opponent processes that result in decreased pharmacologic effect. The body’s adaptation to the medication requires an increased dose to achieve pain relief.
Opioid tolerance may lead to physical dependence, which is described as a neuro-adaption state to a particular opioid medication that results in a physical withdrawal crisis if the medication is abruptly discontinued. Opioid tolerance and dependance differ from the disease of addiction, although patients with opioid addiction also may experience tolerance and dependence.
Collaborate with the healthcare team to evaluate the use of preoperative opioid medication or other adjuvant medications. Abrupt cessation of opioids (such as heroin, hydrocodone, and oxycodone) in patients who are physically dependent may lead to severe opioid withdrawal symptoms. These symptoms typically begin within 6 to 12 hours after a missed dose, peak at 36 to 72 hours, and gradually diminish over the next 4 to 7 days. Patients who have been told to take nothing by mouth for several hours before surgery may present for surgery in mild-to-moderate opioid withdrawal. Symptoms may include nausea, vomiting, piloerection (goosebumps), sweating, tearing, yawning, irritability, and increased pain intensity. Use the Clinical Opiate Withdrawal Scale to assess a patient’s severity of opioid withdrawal.
MAT. Some patients with SUD may be prescribed MAT with buprenorphine, methadone, or naltrexone.
Buprenorphine remains poorly understood by many providers, given its unique pharmacology as a partial µ-agonist or a mixed agonist–antagonist with a high affinity for the µ-receptor. Current literature suggests collaborating with the patient, outpatient prescribing provider, and surgical team (anesthesia, pain management, surgeon, and nursing staff) to consider continuing buprenorphine through the perioperative period. Given the complexity of this medication, an individualized approach is recommended.
Methadone is inexpensive and well-tolerated by many patients with chronic pain and should be continued postoperatively for pain or for maintaining the MAT protocol. Patients receiving MAT with methadone may be treated with supplemental opioid medication if they experience severe pain uncontrolled with other pharmacologic and nonpharmacologic interventions.
Naltrexone blocks the effects of opioids by competitive binding at opioid receptors. Determine which naltrexone formulation the patient is receiving—daily by mouth or monthly by injection. The oral formulation should be held 24 to 48 hours before surgery if any opioids will be administered perioperatively. For patients receiving injections, more detailed planning will be required because continuous dosing lasts up to 4 weeks.
In an emergent surgical situation, regional analgesia or nonopioid analgesics are recommended. If opioid therapy is required, anticipate critical care monitoring and anesthesia provider consultation for postoperative pain management.
Discharge education
Discharge considerations for patients with chronic pain should include education on the safe use of medications, particularly if they have additional opioid medicines at home. Printed and verbal instructions should address adverse side effects of opioid medications, clinical signs of opioid withdrawal, and signs of an opioid overdose.
The U.S. Food and Drug Administration recommends that providers consider co-prescribing naloxone with an opioid prescription for use in case of an overdose. Review the rationale and indications for naloxone use and administration with patients. In addition, provide instructions on how to store and dispose of unused opioid medications, especially when children are in the home.
Leverage your power
Patients with chronic pain have a higher risk for uncontrolled perioperative pain, requiring nurses to be knowledgeable about safe and effective multimodal strategies for pain palliation. The collaborative nature of nursing practice lends itself to leveraging the power of interprofessional teams to create an optimal postoperative pain management plan that incorporates the patient’s voice. Enhance your ability to care for this population by exploring the current literature and adopting patient-centered strategies.
Marie O’Brien is the coordinator of the Integrative Pain Management Program at Mather Hospital Northwell Health in Port Jefferson, New York. Aaron M. Sebach is an associate professor and director of graduate nursing programs at Wilmington University in New Castle, Delaware, and a hospital medicine nurse practitioner at TidalHealth Peninsula Regional in Salisbury, Maryland.
References
Andrews-Cooper IN, Kozachik SL. How patient education influences utilization of nonpharmacological modalities for persistent pain management: An integrative review. Pain Manag Nurs. 2020;21(2):157-64. doi:10.1016/j.pmn.2019.06.016
Coluzzi F, Bifulco F, Cuomo A, et al. The challenge of perioperative pain management in opioid-tolerant patients. Ther Clin Risk Manag. 2017;13:1163-73. doi:10.2147/TCRM.S141332
Delk W, Quinlan-Colwell A. The journey of the American Society for Pain Management Nursing into advocacy and governmental affairs. Pain Manag Nurs. 2020;21(5):395-8. doi:10.1016/j.pmn.2020.06.004
Doan LV, Blitz J. Preoperative assessment and management of patients with pain and anxiety disorders. Curr Anesthesiol Rep. 2020;10(1):28-34. doi:10.1007/s40140-020-00367-9
Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Academies Press; 2011. ncbi.nlm.nih.gov/books/NBK91497
Pasero C, Quinlan-Colwell A, Rae D, Broglio K, Drew D. American Society for Pain Management Nursing position statement: Prescribing and administering opioid doses based solely on pain intensity. Pain Manag Nurs. 2016;17(5):2912. doi:10.1016/j.pmn.2016.08.002
Raja SN, Carr DB, Cohen M, et al. The revised International Association for the Study of Pain definition of pain: Concepts, challenges, and compromises. Pain. 2020; 161(9):1976-82. doi:10.1097/j.pain.0000000000001939
Treede R-D, Rief W, Barke A, et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain. 2019;160(1):19-27. doi:0.1097/j.pain.0000000000001384
United States Department of Health and Human Services. Pain Management Best Practices Inter-Agency Task Force Report: Updates, Gaps, Inconsistencies, and Recommendations. 2019.
Urman RD, Böing EA, Khangulov V, et al. Analysis of predictors of opioid-free analgesia for management of acute post-surgical pain in the United States. Curr Med Res Opin. 2019;35(2):283-9. doi:10.1080/03007995.2018.1481376
U.S. Food and Drug Administration. New recommendations for naloxone. July 30, 2020.
Werner MU, Kongsgaard UE. I. Defining persistent post-surgical pain: Is an update required? Br J Anaesth. 2014;113(1):1-4. doi:10.1093/bja/aeu012
Key words: Perioperative pain management, Chronic pain, Pain management, Evidence-based practice