Quick response to postsurgical complication.
Takeaways:
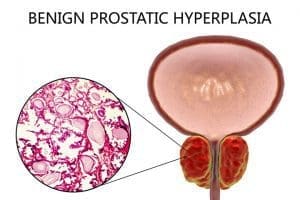
- Benign prostatic hypertrophy, if left untreated, may lead to chronic urinary retention.
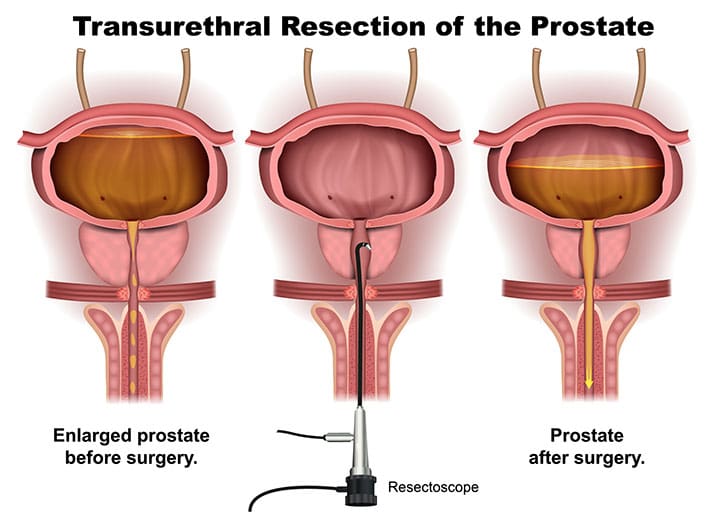
- Medical therapy failure may warrant urologic outflow studies and lead to surgery, such as transurethral resection of the prostate (TURP), to reduce bladder outflow obstruction.
- TURP complications include bladder spasm, urinary incontinence, hemorrhage, and infection.
Martin Denby*, age 70, is admitted to the hospital for transurethral resection of the prostate (TURP) to treat benign prostatic hyperplasia (BPH). He has no cardiac or significant medical history. After surgery, Mr. Denby is transferred to the surgical floor with continuous bladder irrigation (CBI).
History and assessment
After receiving report from the post-anesthesia care unit (PACU) nurse that Mr. Denby’s surgery and PACU stay were uneventful, you assess his orientation and pain level. Mr. Denby’s vital signs are BP 130/84 mmHg, HR 100 beats per minute (bpm), respiratory rate RR 18 breaths per minute, and SpO2 98% on room air; he’s afebrile.
You note that Mr. Denby’s HR is up from the 80s in the PACU. You assess his level of consciousness and document a Glasgow Coma Scale (GCS) of 15/15. At 2:00 pm, you assess his pain level as comfortable (5/10).
On the scene
At 4:00 pm you enter Mr. Denby’s room to obtain vital signs and move him to a chair for dinner. His vital signs are BP 110/78 mmHg, HR 124 bpm, RR 20 breaths per minute, and SpO2 94% on room air. He’s afebrile, and his pain level is 5/10 due to bladder spasms. In addition to the decreased BP and rising HR, you note increased red coloration and a number of dark colored clots in the CBI drainage.
You report your findings to Dr. Jones, Mr. Denby’s urologist. When you re-enter the room, you note Mr. Denby’s color is paler than on transfer to the unit and retake his vital signs: BP 100/76 mmHg, HR 140 bpm, RR 20 breaths per minute, and SpO2 92%. You apply a nasal cannula at 3 L/min and prepare catheter irrigation equipment for Dr. Jones.
Outcome
As Dr. Jones manually irrigates the catheter, removing several clots, Mr. Denby becomes less responsive (GCS 13/15). You call the rapid response team (RRT). The team places Mr. Denby on a cardiac monitor, which shows sinus tachycardia at 142 bpm. Two minutes later, the monitor shows ventricular tachycardia, and he becomes unresponsive, with no pulses. The RRT performs cardiopulmonary resuscitation (CPR) and administers I.V. epinephrine 1 mg, followed by 1 shock and 5 CPR cycles. Mr. Denby converts to sinus rhythm and is transferred to the ICU.
During Mr. Denby’s hospital stay, hand-off reports include vital signs, GCS, and CBI changes. The family receives regular updates.
Education and follow-up
If left untreated, BPH may lead to chronic urinary retention. Initially, medical therapy may be used to treat symptoms. Medical therapy failure may warrant urological outflow studies and lead to surgery, such as TURP, to reduce bladder outflow obstruction. TURP complications include bladder spasm, urinary incontinence, infection, and bleeding.
Patient education should include complications, physical activity limitations, pain control options, and follow-up appointments with the surgeon.
TURP may be perceived as “routine,” but any procedure has complications, as Mr. Denby’s case illustrates. Your quick identification of bleeding and changes in his vital signs and level of consciousness enabled prompt treatment and a positive outcome.
*Names are fictitious.
Norine D. Pulliam is an associate professor in the department of nursing in the College of Health Sciences at West Chester University in West Chester, Pennsylvania.
References
Society of Urologic Nurses and Associates. Benign prostatic hypertrophy: Patient fact sheet. 2019.
Harding MM, Kwong J, Roberts D, Hagler D, Reinisch C. Lewis’s Medical-Surgical Nursing: Assessment and Management of Clinical Problems, Single Volume. 11th ed. Saint Louis, MO: Mosby; 2019.
Key words: Benign prostatic hypertrophy, Continuous bladder irrigation, Transurethral resection of the prostate