Nonsynostotic plagiocephaly is a relatively common craniofacial healthcare concern for pediatric clinicians. Skull asymmetry occurs when an infant’s soft skull becomes flattened in one area, causing a compensatory bulge in another area. It may involve one skull quadrant or up to all four quadrants, and often involves facial bones and neck muscles.
Nonsynostotic plagiocephaly is not related to fusion of skull bones, as is the case in craniosynostosis, a birth defect involving premature synostosis of one or more cranial suture(s). Any asymmetry of the head, face, or neck requires investigation. Asymmetry may be apparent at birth or develop after the first weeks of life. It may persist into adolescence and can be detected in a significant number of adults.
It is a mistake to classify plagiocephaly as a low priority or minor cosmetic issue and not provide early treatment, because the opportunity to intervene occurs while an infant’s skull bones are still moldable. Early recognition of plagiocephaly is important to rule out serious causative factors such as craniosynostosis and neck muscle disorders.
This article presents an overview of plagiocephaly, including a method to quickly screen for asymmetry, explanations of risk factors, interventions, and management, as well as teaching strategies for healthcare providers. The goals are to increase plagiocephaly awareness, screening, and intervention, to reduce the incidence of plagiocephaly, and to improve infant health outcomes.
Newborn positioning and advice
Parents of newborns usually receive advice on supine positioning, but may not receive specific instruction on how to rotate their baby’s head to improve or avoid plagiocephaly. Infant positioning is a primary aspect of national safe sleep recommendations. To reduce the incidence of skull deformity, the American Academy of Pediatrics (AAP) encourages clinicians to provide the following preventive counseling to parents:
- Start the supine position at birth or within a few hours.
- Rotate the infant’s head side-to-side while supine.
- Rotate the infant’s position in the crib.
- Provide exercise and tummy time.
- Reduce time spent restricted in sitting devices.
- Continue positioning up to age 1, even after the infant self-positions.
Parents and caregivers may not be aware of plagiocephaly, or that positioning is most effective while skull bones are moldable starting at birth and during the first months of life. A 2015 nationally representative survey by Eisenberg and colleagues quantified advice received by 1,031 new mothers from four sources (doctors, nurses, family, and media) on five infant-care practices (breastfeeding, sleep position, sleep location, immunization, and pacifier use). Breaking out the results on advice about sleep position, the survey found that doctors and nurses provide advice consistent with recommendations just over 50% of the time. Therefore, nearly 50% of the time important information about sleep position is not being given to patients. Advice influences infant care practices, and infants benefit when parents and caregivers receive and follow advice consistent with recommendations.
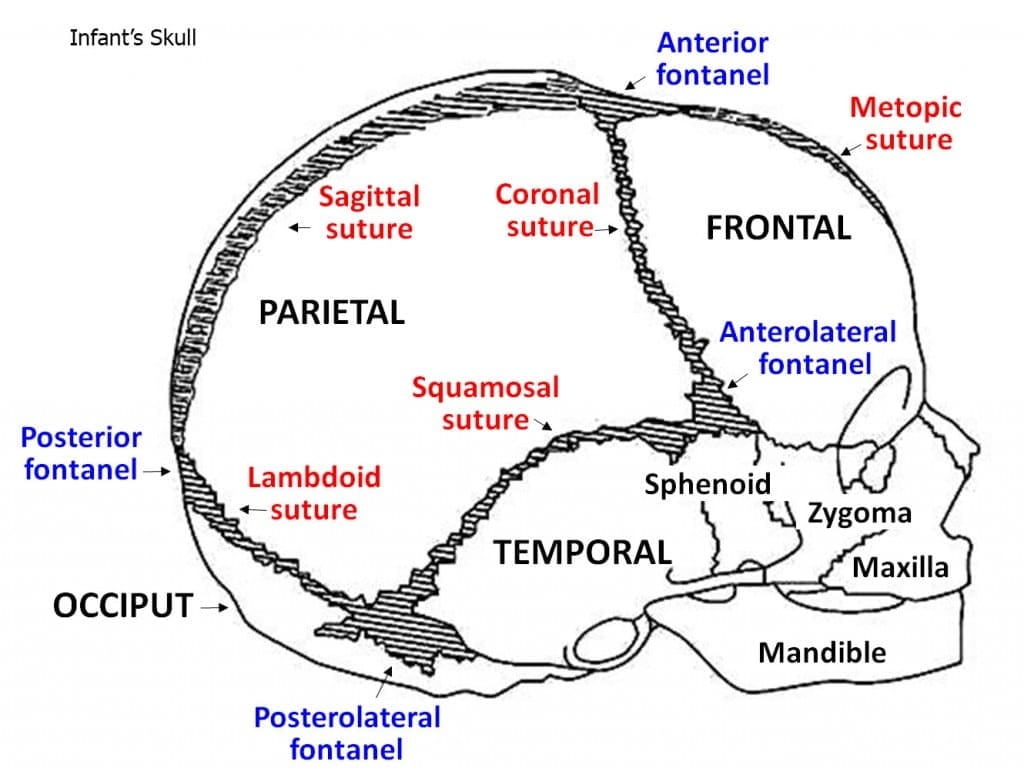
Infant skull structures
Infant skull structures include bone plates, facial bones, sinuses, fibrous sutures, and fontanels, as well as cranial and neck muscles, cartilage, joints, and fibrous connective tissue. (See Infant’s skull.) Neurocranial growth is largely determined by brain growth, with the fastest growth occurring between birth and 90 days. Cranial growth begins to slow at 7 to 8 months old, and cranial sutures are generally interlocked at 24 months old.
Asymmetry screening
Plagiocephaly is determined primarily by clinical evaluation and health history. Incorporate screening into the physical examination; for example, when measuring head circumference look for prominent (bossed) or flattened areas, and when palpating fontanels also palpate sutures for ridging or closure. Head circumference is not an indicator of head shape deformity.
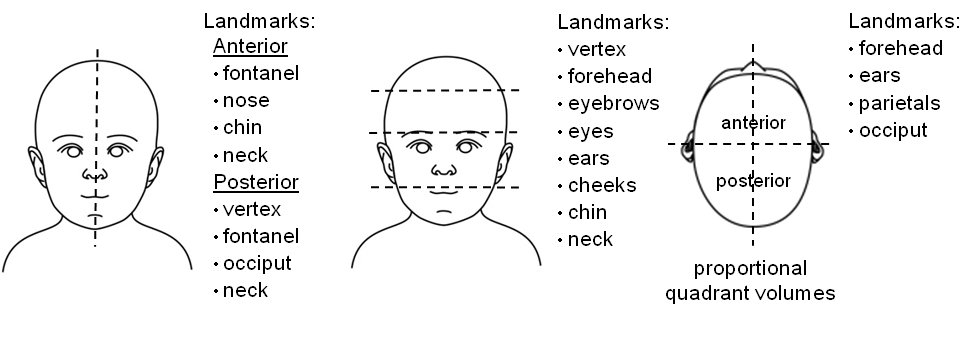
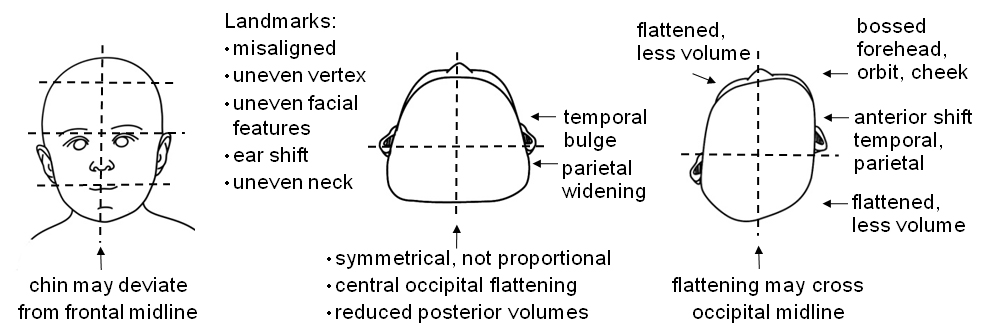
Asymmetry may be subtle. (See Symmetry versus asymmetry.) Visualize alignment by imagining lines that connect features on the head, face, and neck (anterior and posterior, vertical and horizontal). Visualize proportion by dividing the skull into quadrants, noting if quadrant volumes are relatively equal. Finally, document asymmetry: head and face (bossed, flat, uneven, or misaligned areas), and neck (head tilt, shoulder hike, face rotation, reduced range of motion).
Symmetry versus asymmetry
Symmetry
Asymmetry
The illustrations of asymmetry depict only prominent examples of asymmetry, not all possible combinations.
A more precise diagnosis of plagiocephaly includes cranial measurements, severity assessment scales, and photographs or a three-dimensional scan. The AAP recommends early and regular head and neck screening up to age 1. (Click to download Quick screen for Infant Head/Face/Neck Asymmetry.)
Risk factor overview
Risk factors for plagiocephaly are individual, and may be intrinsic, extrinsic, or both. Intrinsic factors affect the growth, size, weight, shape, and patency of skull structures and their ability to accommodate movement, and thus can affect head shape. Intrinsic factors are genetic or congenital (not modifiable); examples include gender (higher incidence in males), gene or chromosome anomaly, prenatal exposure to alcohol or certain medications, or neuromuscular delay. Extrinsic factors are acquired (modifiable). Examples include prolonged immobility, restricted movement, improper positioning, overuse of sitting devices, cultural practices, or lack of awareness about plagiocephaly. Correlated obstetric risk factors include primiparity, plurality, intrauterine position, and assisted delivery. Infants in neonatal care units are at risk because of intrinsic factors, extrinsic factors, or both.
The causes of plagiocephaly may be multifactorial. For example, the supine position (extrinsic) increases extracranial occipital pressure; however, susceptibility to subsequent bone deformity may be related to other unknown factors both intrinsic and extrinsic. The supine position is credited with reducing the incidence of Sudden Infant Death Syndrome (SIDS) by 50%, but is also cited as a factor in the estimated 600% coincident increase in reported cases of plagiocephaly.
Craniosynostosis
Serious risk factors for plagiocephaly include craniosynostosis and neck muscle disorders. Craniosynostosis is the premature closure of one or more cranial suture(s); ossification can occur at points or along the entire suture line. It can be life threatening and requires immediate intervention and often corrective surgery to allow for proper neurocranial growth. Correlated risk factors for craniosynostosis include intrinsic growth factors, autosomal gene expression, certain syndromes, compression forces in utero, older maternal age, maternal medications (clomiphene citrate, fluoxetine, valproic acid, levothyroxine), prenatal diet, or exposure to a teratogen. Signs may include asymmetry of the head, face, or neck, fontanel bulging or premature closure, proptosis, prominent scalp veins, ridging along the affected suture, symptoms associated with increased intracranial pressure (crying, emesis, apnea, seizures), developmental delay, or congenital anomalies. Diagnostic imaging tests include radiography, computed tomography, magnetic resonance imaging, and less often ultrasonography. Craniosynostosis is a reportable birth defect (1 in 2000 U.S. live births); the majority of cases occur in males, are sporadic, non-syndromic, and without family history.
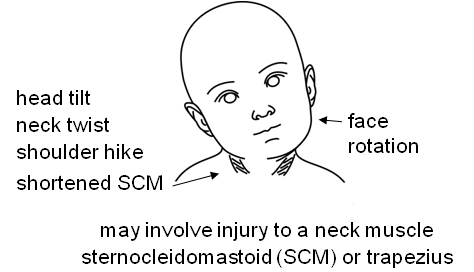
Neck muscle disorders
Neck muscle disorders such as torticollis decrease head and neck movement, interfere with motor milestones, increase the risk of a torticollis-plagiocephaly sequence, and thus require early intervention. Torticollis may be congenital or acquired, and often involves a muscle injury (nerve, vascular, muscular), which results in a shortened neck muscle (sternocleidomastoid or, less often, trapezius). Signs may include head tilt with neck twist, shoulder hike on the affected side, face rotation to the opposite side, and reduced range of motion. (See Neck asymmetry.) The infant may exhibit a preference for one side, or be unable to rotate the head 90 degrees (chin over shoulder) on the affected side. Torticollis treatment includes neck exercises or physical therapy and, rarely, surgery in cases resistant to therapy. Congenital muscular torticollis is an independent factor in the failure of conservative treatment for plagiocephaly.
Neck asymmetry
Intervention and management
Conservative treatment guidelines for skull deformity include: preventive counseling (anticipatory guidance), mechanical adjustments and exercise (positioning, tummy time, physical therapy), and referral as needed. For torticollis, teach neck exercises or refer for physical therapy.
For plagiocephaly, a 2- to 3-month trial of positioning is recommended, although correction may require more time. For asymmetry that does not improve or if there are any concerns, refer to a craniofacial specialist. If craniosynostosis has been ruled out, subsequent management may include continued conservative treatment, a cranial device, or, rarely, surgery in cases refractory to treatment. Risk factors for conservative treatment failure include older infant age, parental noncompliance, severity of deformity, craniosynostosis, torticollis, or neuromuscular developmental delay. Because plagiocephaly may involve intrinsic factors, parents may position their infant properly without improvement of asymmetry. Steinberg and colleagues demonstrated in one large (n = 4,378), well-controlled study, that 77.1% of asymmetrical skulls related to positional deformity normalized with conservative treatment.
Cranial devices are approved and regulated by the Food and Drug Administration (FDA) and require a prescription. For infants in neonatal care units, one approved cranial device is an adjustable gel-filled head wrap designed to alleviate extracranial pressure related to prolonged immobility that may cause skull asymmetry. For older infants, cranial helmets or molding orthoses provide passive resistance to channel skull growth, and are custom-designed based on the infant’s head measurements. The FDA approves helmets for use between age 3 and 18 months; however, the effectiveness of helmet therapy depends on cranial growth (which slows after age 7 to 8 months). The AAP recommends intervention while the skull bones are still malleable between ages 4 and 12 months. Some insurance providers require helmet intervention before age 12 months because of decreased cranial growth, plus documentation of a 2- to 3-month trial of positioning without improvement of asymmetry. Risk factors for helmet therapy failure include late age of initiation, parental noncompliance, or the presence of torticollis or developmental delay.
Educational strategies for parents and providers
Teach safe positioning along with existing safe sleep education programs in the prenatal, hospital, and clinic settings. Develop standardized information to help clinicians provide advice that is consistent with national recommendations as well as to minimize personal bias. A combination of teaching methods is best for adult learners: auditory (verbal instructions, question-answer, feedback), kinesthetic (demonstration, hands-on practice), and visual (video, written instructions, and learning materials translated into the parent’s language). Video is especially effective, as are commitment pledges signed by the parents, based on 6-month follow-up knowledge-retention surveys. Consider a brief follow-up survey to collect metrics on the effectiveness of the education program you use.
Demonstrate head positioning using the infant or a doll, and reinforce learning with hands-on practice. Prepare parents to teach positioning to other family members and caregivers. Discuss methods to encourage early infant movement: provide clothes that protect but allow freedom to move (sleep blankets); limit use of blankets and swaddles that restrict movement; limit time restricted in sitting devices (car seats, strollers, swings, carriers) and walking devices; rotate sides for feeding and holding; rotate between supine and prone positions during playtime; and provide activities that promote turning and reaching movements.
Anticipate and address concerns parents may encounter. For example, parents may worry about touching the “soft spot” or that turning the baby’s head will hurt; parents may feel guilty, embarrassed, judged, or worried about their child’s future body image. Some parents report a “flat spot” to clinicians but are advised not to worry and to “wait and see,” or may be told the baby will grow out of it or that their hair will cover it, and thus stop follow-up.
Ask questions to determine the parents’ level of knowledge. The following examples of questions and anticipatory guidance are based on the format used in the AAP Bright Futures guidelines.
Questions to ask parents and caregivers:
- Do you know why babies are placed on their back to sleep?
- What do you know about SIDS?
- Do you know why babies have fontanels or “soft spots”?
Anticipatory guidance:
- It’s important to place baby safe to sleep on his back, not tummy or side, and to rotate his head.
- Let’s rotate baby’s head while she is asleep.
- Show me how you will demonstrate the baby’s positioning to your family.
Parents may ask whether there are health risks related to plagiocephaly. International evidence-based research correlates plagiocephaly with risks to oral, sensory, and developmental health outcomes. The AAP does not acknowledge causal links between positional skull deformity and vision problems or mandibular asymmetry. However, some insurance policies cite evidence-based research that correlates plagiocephaly with future ocular abnormalities, oral abnormalities, or both. In all cases of plagiocephaly, early intervention and close monitoring are prudent to improve children’s health outcomes.
Early action essential
Plagiocephaly is common, so be prepared for cases when presented. Screen for and recognize asymmetry; intervene early and refer as needed; educate parents/caregivers, provide advice consistent with recommendations, and follow all safe sleep guidelines; and model a culture of safe sleep within the prenatal, hospital, and pediatric healthcare settings. Improved plagiocephaly outcomes involve early intervention and regular communication between the team players, the infant’s parents and caregivers, the primary care team, and the allied specialists. Pediatrics requires team play.
Selected references
American Academy of Pediatrics. Bright Futures. Recommendations for Preventive Pediatric Health Care Periodicity Schedule. May 2015. www.aap.org/en-us/professional-resources/practice-support/Pages/PeriodicitySchedule.aspx
Eisenberg SR, Bair-Merritt MH, Colson ER, Heeren TC, Geller NL, Corwin MJ. Maternal report of advice received for infant care. Pediatrics. 2015;136(2):e315-e322.
Goodstein MH, Bell T, Krugman SD. Improving infant sleep safety through a comprehensive hospital-based program. Clin Pediatr. 2015;54(3):212-221.
Healthnet National Medical Policy NMP311. Plagiocephaly treatments, dynamic orthotic cranioplasty and soft helmets. March 2015. www.healthnet.com/portal/provider/content/iwc/provider/unprotected/working_with_HN/content/medical_policies.action
Holland D, Chang L, Ernst TM, et al. Structural growth trajectories and rates of change in the first 3 months of infant brain development. JAMA Neurol. 2014;71(10):1266-1274.
Kaplan SL, Coulter CP, Fetters L. Physical therapy management of congenital muscular torticollis: an evidence-based clinical practice guideline. Pediatr Phys Ther. 2013;25:348-394.
Laughlin J, Luerssen TG, Dias MS. AAP Committee on Practice and Ambulatory Medicine, Section on Neurological Surgery. Prevention and management of positional skull deformities in infants. Pediatrics. 2011;128(6):1236-1241.
Looman WS, Flannery AB. Evidence-based care of the child with deformational plagiocephaly, part 1: assessment and diagnosis. J Pediatr Health Care. 2012;26:242-250.
Moon RY. AAP Task Force on Sudden Infant Death Syndrome (AAPTFSIDS). SIDS and other sleep-related infant deaths: expansion of recommendations for a safe infant sleeping environment. Pediatrics. 2011;128(5):1030-1039.
Ridgway EB, Weiner HL. Skull deformities. Pediatr Clin North Am. 2004;51:359-387.
Seruya M, Oh AK, Taylor JH, Sauerhammer TM, Rogers GF. Helmet treatment of deformational plagiocephaly: the relationship between age at initiation and rate of correction. Plast Reconstr Surg. 2013;131(1):55e-61e.
Steinberg JP, Rawlani R, Humphries LS, Rawlani V, Vicari FA. Effectiveness of conservative therapy and helmet therapy for positional cranial deformation. Plast Reconstr Surg. 2015;135(3):833.
Texas Department of State Health Services. Birth Defects Epidemiology & Surveillance. Birth Defect Risk Factor Series: Craniosynostosis. Aug 2011. www.dshs.state.tx.us/birthdefects/risk/risk-craniosynostosis.shtm
United Healthcare Medical Policy. Plagiocephaly and craniosynostosis treatment. Policy No. 2015T0031M. Oct 2015. www.unitedhealthcareonline.com/ccmcontent/ProviderII/UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesPdf/Tools%20and%20Resources/Policies%20and%20Protocols/Medical%20Policies/Medical%20Policies/Plagiocephaly_and_Craniosynostosis_Treatment.pdf
Laura C. Steinmann is a consultant at Steinmann Prosthetics & Orthotics in Las Cruces, New Mexico.