This innovative model can help expand access.
- Some of the current nursing workforce stress stems from inadequate support and the demands of an aging population.
- Project ECHO is a collaborative learning model that connects rural clinicians with an interprofessional team of specialists via videoconferencing.
- Using an “all teach, all learn” approach, Project ECHO offers interactive education, peer-to-peer learning, case co-management, and collaborative problem-solving.
The American Nurses Association reports that many factors influence the current workforce strain on nursing, including inadequate support and the demands of an aging population, many with advanced chronic conditions. In The Future of Nursing 2020–2030: Charting a Path to Achieve Health Equity, the National Academy of Medicine promotes an interprofessional approach to education and training for nurses to help develop their leadership skills as well as their understanding of health equity, social determinants of health, and population health. Interprofessional geriatrics training opportunities for nurses can address the diverse and complex healthcare demands of older Americans. (See Geriatric care challenges.)
The University of North Texas Health Science Center (UNTHSC), in Fort Worth, implemented Project ECHO (Extension for Community Healthcare Outcomes), a collaborative learning model that originated at the University of New Mexico. Project ECHO connects rural clinicians in primary care and long-term care settings with an interprofessional team of specialists via videoconferencing sessions. Using didactic presentations and case-based learning, these experts answer real-world questions.
Dumped: When nursing homes abandon patients to the hospital
Geriatric assessment: Essential skills for nurses
Preventing polypharmacy in older adults
Geriatric care challenges
Older adults make up the fastest growing cohort in the United States. The U.S. Department of Health and Human Services anticipates over 80 million older adults by the year 2040. This unprecedented growth requires a healthcare workforce qualified to manage the complexities of chronic illnesses, comorbidities, cognitive disorders, and social factors.
Many within this population reside in rural areas, which stretches an already challenged eldercare workforce. According to the Health Services and Resources Administration, rural communities make up 65.83% of the primary medical health professional shortage areas. The anticipated decrease in geriatricians over the next decade requires more geriatrics-trained healthcare professionals, as well as an increased reliance on interprofessional models of care to maximize the existing workforce.
How the project works
UNTHSC became an ECHO Hub site in 2019 with the creation of a Geriatrics ECHO line targeting rural primary care practices caring for older adults. A second ECHO line for long-term care facility teams (Nursing Home STRONG ECHO) began in 2020. Project ECHO’s “All teach, all learn” approach has four primary elements: interactive education, peer-to-peer learning, case co-management, and collaborative problem-solving. The dedicated UNTHSC Project ECHO team includes a medical director, a program coordinator, and a team of interdisciplinary geriatric care experts. Specialty team members currently consist of four geriatricians, a psychiatrist, two nurse practitioners (NPs), a physical therapist, a public health infection-control preventionist, a licensed clinical social worker, and a clinical pharmacist.
Participation
We invited community health professionals to attend hour-long sessions focused on learning about the healthcare needs of older adults. Our Project ECHO website includes general information and a link to register for Geriatric ECHO or Nursing Home STRONG ECHO sessions. After registration, participants received a monthly reminder email with a Zoom link. Each session offered free continuing education credit; instructions for claiming credit were sent by email at the end of each session. The participant could opt out at any time. We used online participant surveys to collect data that aid programmatic assessment and curricular planning.
We recruited participants via social media, mailing campaigns, and word of mouth. Initially, we focused our marketing efforts in Texas because of its geographic proximity, established community relationships, and large population of rural providers. We then expanded our efforts to include regions surrounding Texas. In addition to these targeted marketing and advertising efforts, participants can attend from across the country and around the world.
Sessions
Each session, which follows the nationally acclaimed ECHO model, comprises a brief didactic presentation by a content expert, followed by a case presentation by a participant. The remainder of the session allows for questions and discussion among participants. This unique learning environment allows everyone to act as a teacher and a learner.
ECHO sessions follow two primary scheduling approaches—a time-limited or an ongoing series. Time-limited series enrollment occurs before the session begins; participants are encouraged to prioritize attending all sessions as the topics may build upon each other. An ongoing series has rolling enrollment; participants can join at any time and attend as frequently as they’re able.
The UNTHSC Project ECHO team has scheduled sessions in both formats depending on the needs of the audience and curricular goals. For example, each year we provide a six-session series on dementia. A dementia diagnosis creates uncertainty for patients and their caregivers, who frequently turn to their primary care providers for help. The six sessions in this series include information paired with real-life experience to better equip healthcare teams to provide essential, person-centered guidance. The Nursing Home STRONG ECHO line has created a virtual community of long-term care teams with regularly scheduled sessions. Topics continue to evolve as needed for the audience. In 2023, the focus shifted away from COVID-19 and toward emergency preparedness.
How we collected data
We used online participant surveys to collect data. Participants provided basic demographic information at registration and responded to requests for feedback after completing sessions. We also requested job titles, credentials, health center names, and addresses. The Geriatrics ECHO data consist of information from September 2019 to May 2022; the Nursing Home STRONG ECHO, from November 2020 to September 2022 (which includes Agency for Healthcare Research and Quality [AHRQ] COVID-19 Action Network ECHO sessions held from November 2020 to August 2021).
Interviews with participants, as well as feedback received during ECHO sessions, provided qualitative data on participant experience. Prior participant case presentation submissions offered supporting background information.
Quantifying project impact
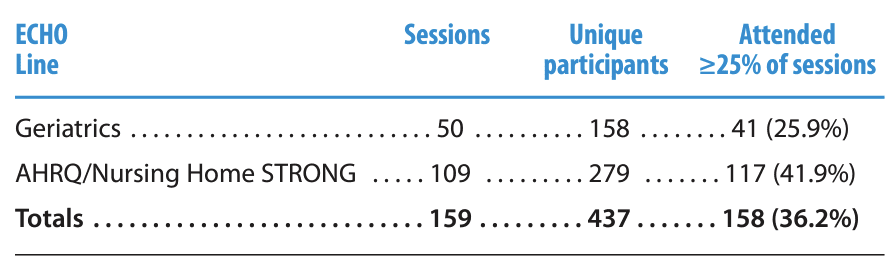
Between September 2019 and September 2022, the two UNTHSC ECHO lines offered 159 sessions. A total of 437 unique participants attended the sessions, including 158 in the Geriatrics ECHO and 279 in the AHRQ/Nursing Home STRONG ECHO. Although the Geriatrics ECHO line averaged more unique participants per session, more participants attended at least 25% of the AHRQ/Nursing Home STRONG ECHO sessions for a given program series (n=117, 41.9%). Overall, 158 (36.2%) participants attended at least 25% of sessions for a given program series.
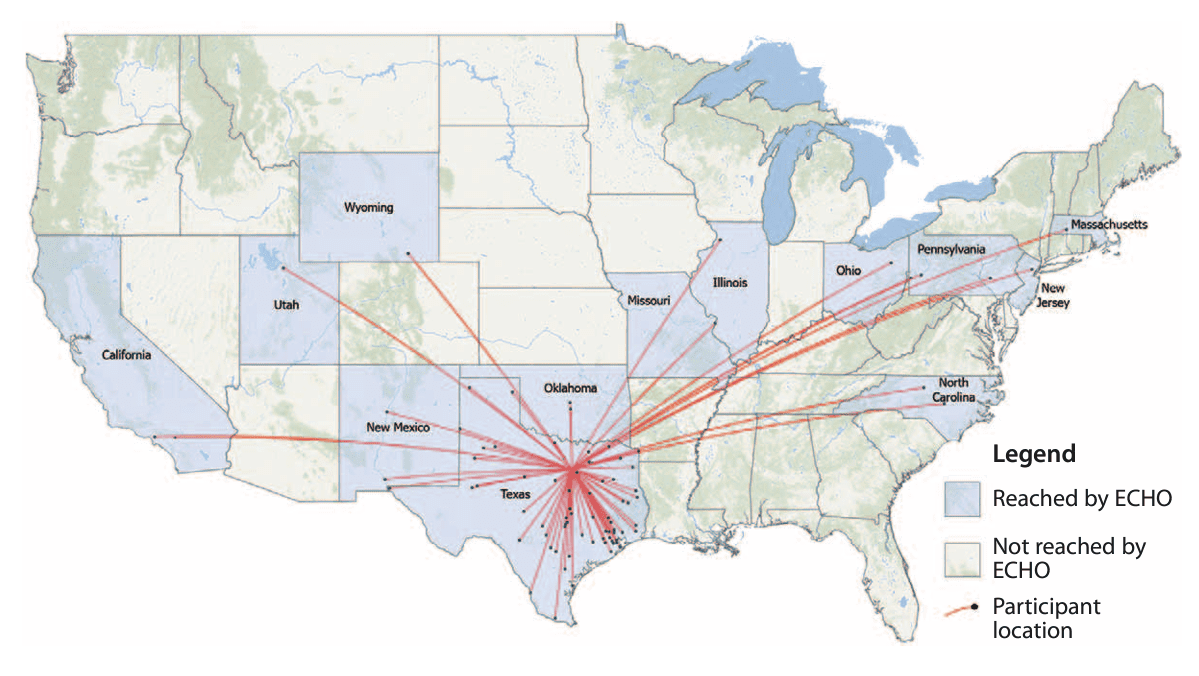
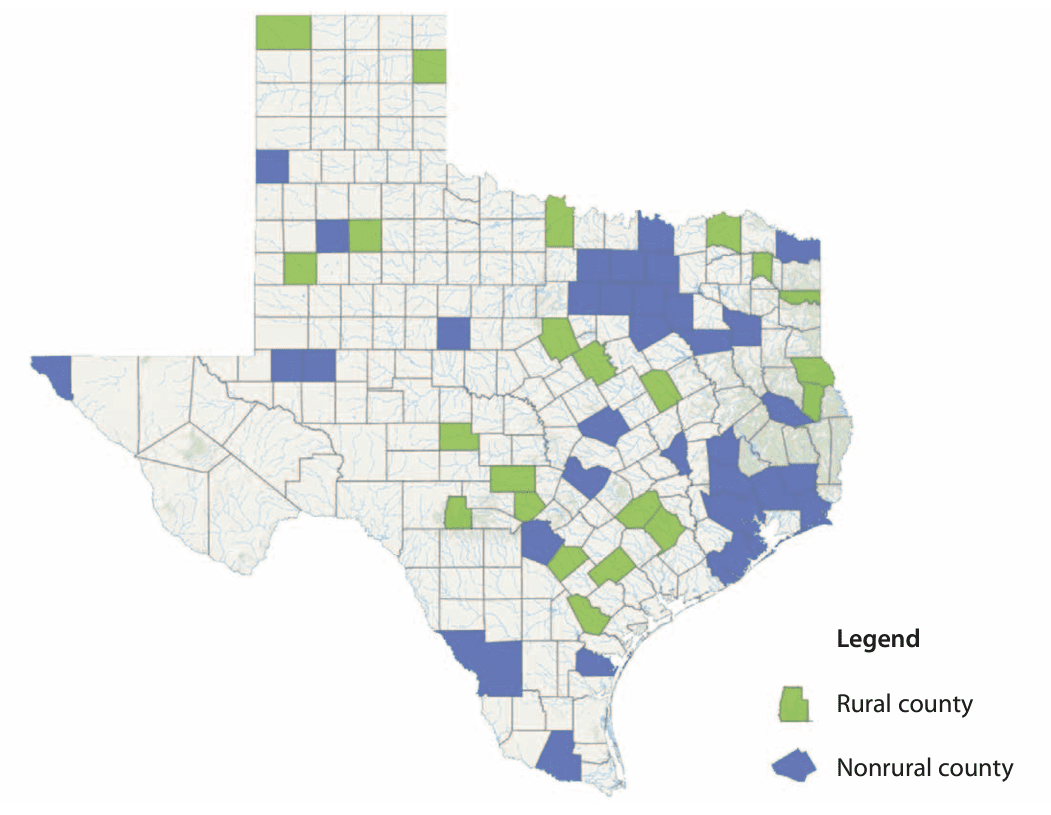
The ECHO lines reached a total of 14 states and 77 unique counties within those states (23 of those counties are considered rural). In addition, the Geriatrics ECHO included participants from Myanmar and Nepal. The ECHO lines reached 58 unique counties within Texas, with 22 counties considered rural.
Most participants reported their job title as nurse (including director of nursing, assistant director of nursing, and RN). Overall, nurses accounted for 128 (36.2%) of the 354 participants who reported a job title. The most common participant job title in the Geriatrics ECHO line was physician (n=38, 39.6%); in the AHRQ/Nursing Home STRONG ECHO it was nurse (n=105, 40.7%). Other commonly reported job titles included administration, leadership, and student. Several student participants were NP students. Nine advanced practice practitioners (most NPs) attended. (See Participants and project reach.)
Participants and project reach
A single Microsoft Excel spreadsheet analyzed participant data from all sessions into various data points with a specific focus on the number of unique participants, the location, and the job title. Participants who attended 25% or more of sessions for a given program series provided additional data on the perspective of returning participants.
Using ArcGIS, a geographic information systems software that analyzes geospatial data, we imported participant ZIP codes and then created maps. The following map depicts the hub-and-spokes pattern of geographic locations (including 14 states) reached by Project ECHO from September 2019 through September 2022. Locations that participated but aren’t shown in this map include Alaska, Myanmar, and Nepal.
The following map depicts Texas counties reached by the UNTHSC Project ECHO lines, divided into rural and nonrural. Of the 58 Texas counties, 22 (37.9%) were considered rural (based on the U.S. Office of Management and Budget’s classification). In general, these counties lack an urban core or have an urban core of less than 50,000.
Participant experience
A portion of each ECHO session focused on problem-solving a real patient case presented by a participant. Case presenters provided a summary of the patient or scenario and a question they wanted help answering, such as the following:
- How can I help this patient take their medication correctly?
- What are the next best steps to control their pain?
- What is the best approach to manage their osteoporosis?
- What are other options for their anxiety?
- How do you transition a patient with progressive dementia to a safer living environment when the patient refuses to leave their home?
- What antidepressant would you try next for this patient?
Case example 1
Carrie, a primary care NP, appreciated the ECHO team’s support in caring for an older adult with anxiety and dependence on benzodiazepines. Carrie’s 78-year-old patient had been taking alprazolam for years. The patient had longstanding anxiety and more recently had experienced falls and complaints of memory loss. Carrie recognized the potential benefits of stopping alprazolam and had an initial discussion with the patient. The patient agreed to try something different for anxiety, and Carrie came to the Geriatrics ECHO for input.
The participants helped Carrie develop a plan to wean the patient off alprazolam gradually and use alternative medications and therapeutic approaches for symptom management. Carrie learned about resources to support both patients and practitioners, such as deprescribing.org, and left the session with a plan for the next steps.
Case example 2
Angela, a director of nursing at a skilled nursing facility, joined the Nursing Home STRONG ECHO to hear a presentation on employee retention and recognition. In Angela’s feedback, she said that the group discussion helped individuals feel connected to others facing similar challenges in their facilities. Angela felt that suggestions shared during the didactic session and group discussion validated leadership practices and provided direction for new ways to show team appreciation and recognition.
Project outcomes
In the past 3 years, the Project ECHO model at UNTHSC has proven effective in reach and scalability. Participants include a diverse range of individuals from the nursing profession (students, novices, proficient nurses) with varied education (vocational, undergraduate, graduate). The creation of a virtual community with diversity of experience provides a unique learning opportunity for everyone. The UNTHSC ECHO Hub team learns from the participants, and the participants enjoy the solidarity and connection of the community.
UNTHSC found the Project ECHO model to be cost-effective. After receiving approval as an official Project ECHO Hub, UNTHSC outfitted an existing conference room with the necessary equipment (cost under $4,000) as specified by the ECHO Institute. Because of our hub status, the ECHO Institute provided access to their proprietary database and Zoom account. The hub’s organizational and coordinating staff created the curriculum based on the needs of the target audience. Team members and staff required for coordination and recruitment varied in size and scope depending on the focus and frequency of the ECHO sessions.
Facilitate learning
The Project ECHO model produces an effective and efficient platform to facilitate interprofessional learning by assembling experts and learners from various geographical locations, both urban and rural. By eliminating travel time and expense, participants, especially NPs in rural practices, can easily connect with colleagues and acquire specialty knowledge. Should the removal of scope-of-practice restrictions for NPs and expansion of payment eligibility for Medicaid occur, as recommended by the Institute of Medicine, creative approaches such as Project ECHO present a relevant, cost-effective, and scalable avenue for interprofessional geriatrics training to a range of settings.
For nurses and nursing home leadership, Project ECHO provides a forum to connect with fellow leaders and learn about relevant care models, as well as changing policies and regulations that impact residents, families, and staff. During the height of the COVID-19 pandemic, our Nursing Home STRONG ECHO provided a weekly source of information to address the ever-evolving landscape of infection prevention and control and reporting requirements. As we emerge from the pandemic, our interactive ECHO sessions facilitate an exchange of best practices for managing changing regulations, policies, and treatment options while also maintaining quality care for nursing home residents and enhancing staff morale for workforce retention.
The discussion of real-life scenarios in both ECHO lines addresses complex healthcare issues within a context that fosters whole health, health equity, and leadership. One of the many benefits of Project ECHO is the development of a healthcare workforce competency to meet the rising demands and complexities of an aging population. Project ECHO also helps to promote professional growth, stave off burnout, and increase job satisfaction.
Acknowledgement: This project was supported by the Health Resources and Services Administration of the U.S. Department of Health and Human Services as part of a Geriatrics Workforce Enhancement Program under grant number UTQHP28735. The North Texas Regional Institutional Review Board approved the study as meeting criteria for exempt status.
Learn more
To learn more about Project ECHO, tap into the following resources:
- The ECHO Institution provides an excellent overview of the program: hsc.unm.edu/echo</li>
- To explore topics offered through existing ECHO Hub sites, visit the ECHO Hubs dashboard and search by focus areas: hsc.unm.edu/echo/partner-portal/data-marketplace/interactive-dashboards
- To become a Hub site, visit the Become a Partner page: hsc.unm.edu/echo/become-a-partner
The ECHO Institute holds monthly introductory sessions to help potential partners decide whether the ECHO model is right for them. Additional partner training courses—offered in-person and virtually at no charge—help organizations understand and properly implement the ECHO model. The ECHO Institute also provides partners with access to its proprietary database and Zoom account.
Kate Taylor is assistant dean of clinical and outreach affairs at the College of Nursing University of North Texas Health Science Center (UNTHSC), an assistant professor in internal medicine and geriatrics at the Texas College of Osteopathic Medicine, and clinical executive for SaferCare Texas. Sarah Ross is an associate professor in the Texas College of Osteopathic Medicine. Susanna Luk-Jones is the research budget director for the Center for Older Adults at UNTHSC. Matthew Biggerstaff is a master of public health and medical student at Texas College of Osteopathic Medicine.
American Nurse Journal. 2023; 18(12). Doi: 10.51256/ANJ122323
References
Administration for Community Living. 2021 profile of older Americans. U.S. Department of Health and Human Services. acl.gov/sites/default/files/Profile%20of%20OA/2021%20Profile%20of%20OA/2021ProfileOlderAmericans_508.pdf
American Geriatrics Society. Geriatrics workforce by the numbers. americangeriatrics.org/geriatrics-profession/about-geriatrics/geriatrics-workforce-numbers
American Nurses Association: Nurses in the workforce. nursingworld.org/practice-policy/workforce/
Barnes H, Richards MR, McHugh MD, Martsolf G. Rural and nonrural primary care physician practices increasingly rely on nurse practitioners. Health Aff. 2018;37(6):908-14. doi:10.1377/hlthaff.2017.1158
Brown T, Miller Temple K, Rudolphi J. NRHA policy paper: Rural America’s senior citizens: Considerations for transportation, healthcare access, connectedness, nutrition and economics. National Rural Health Association. 2020. www.ruralhealth.us/NRHA/media/Emerge_NRHA/Advocacy/Policy%20documents/2020-NRHA-Policy-Document-Rural-America%E2%80%99s-Senior-Citizens.pdf
U.S. Department of Health and Human Services. Designated health professional shortage areas statistics. September 30, 2023. data.hrsa.gov/topics/health-workforce/shortage-areas
National Academy of Medicine. The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity. Washington, DC: The National Academies Press. nap.nationalacademies.org/catalog/25982/the-future-of-nursing-2020-2030-charting-a-path-to
Rowe JW. The US eldercare workforce is falling further behind. Nat Aging. 2021;1(4):327-9. doi: 10.1038/s43587-021-00057-z
Texas Commission on the Arts. Rural Texas counties. www.arts.texas.gov/initiatives/rural-initiatives/rural-texas-counties/
U.S. Department of Health and Human Services. Defining rural population. June 2020. hhs.gov/guidance/document/defining-rural-population
Key words: geriatric healthcare, long-term care, Extension for Community Healthcare Outcomes, collaborative care, rural settings, videoconferencing