Are you using the wrong kind of medical tape on your patients? Although we strive to provide the safest care possible, some nurses may not realize that medical tape used to secure tubes and dressings can cause harm. The harm may stem from using the wrong product or using a product incorrectly, which can cause adhesive failure or skin injury.
Many different medical tapes are available. To prevent injury, you need to choose the right tape for each patient. But knowing which tape is right can be challenging even for experienced nurses. To choose and use tape successfully, you need to understand the components of medical tape and base tape selection on your patient assessment findings.
Medical tape has three jobs—to provide an initial stick, increase adhesion, and remain intact. The initial stick isn’t sufficient for the tape to stay in place. To improve adhesion, you must apply pressure. Tape must stay intact, but oil and emollients can separate the adhesive from the backing or from the patient’s skin. Using an emollient product, such as an adhesive remover or lotion, can help you remove tape without injuring the skin.
For tape to serve its purpose, the product you choose must suit ambient conditions. For example, moisture can prevent the adhesive from securing to the skin; oil from sebaceous glands may cause tape to fail and peel off.
Tape-related injury
Medical adhesive-related skin injury (MARSI) occurs when tape causes stripping, separation, or tearing of the epidermal layers. Erythema can occur when you remove tape from the skin. Stripping may occur when the tape is stronger than the skin layers, causing removal of superficial dermal layers on tape removal. Blisters may form if you apply tape with tension and the product restores its shape but pulls apart epidermal layers. Tears can occur when you apply or remove tape with tension or if friction arises, causing skin layers to separate.
Tape components
Although not all medical tapes are alike, all of them are pressure-sensitive adhesives. Tape is a combination of backing and adhesive; we activate the adhesive by applying pressure—for instance, when we rub the tape on the patient’s skin. Warmth promotes contact of the tape to the skin’s irregular surface.
The combination of backing and adhesive determine a tape’s qualities. The variety of adhesives and backings available offers an array of products designed to excel under specific conditions.
Backing
Tape backing can be paper, cloth, foam, or another material. These materials vary in strength, water resistance, breathability, and stretch. (See the box below.)
Adhesive
Adhesive is the glue that enables the backing to stick and do its job. Medical tapes have acrylate or silicone adhesives.
- Acrylate is a low-sensitizing adhesive and works with a variety of backings. Incorrect use can result in MARSI. Not all acrylate tapes are the same; some have a higher initial adhesion on damp skin, whereas others have increased adhesion over time.
- Silicone, a newer adhesive, is gentle and conforms easily to the skin’s surface. Its gentleness allows for easy removal but not the strength needed to secure critical tubing.
Assessing the patient
To choose the right tape for your patient, start by assessing your patient. First, examine the skin at the site where you’ll secure the tape. Look for hair and sebaceous and sweat glands there, as these may impair tape adhesion.
Next, determine if your patient has moist, dry, or fragile skin. The skin’s condition helps you decide if you must use a tape that breathes, removes gently, or secures firmly.
Consider the tape’s purpose. For example, if you need to secure an endotracheal tube on a moist face, the tape must be able to stay intact and secure; in this case, cloth tape might be best. In contrast, a dressing on a moving joint needs a tape that stretches and accommodates for movement, such as a foam or soft cloth tape. Your assessment findings help you decide whether to use a tape that stretches, breathes, or repels moisture.
Next, evaluate for potential stressors, such as tension, flexion, friction, and movement. These influence product selection because you want to avoid separation of the epidermal layers, peeling of dressings, and tube dislodgement.
In some situations, a patient may have fragile skin but require a strong tape; examples include neonates, older adults, and patients with edematous skin. See the box below for tips on how to manage problems commonly encountered when using medical tape.
Managing tape-related problems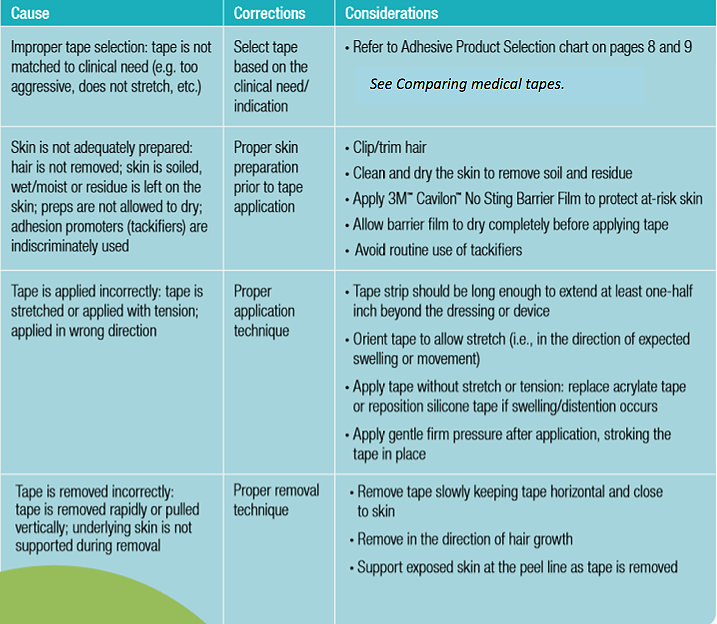 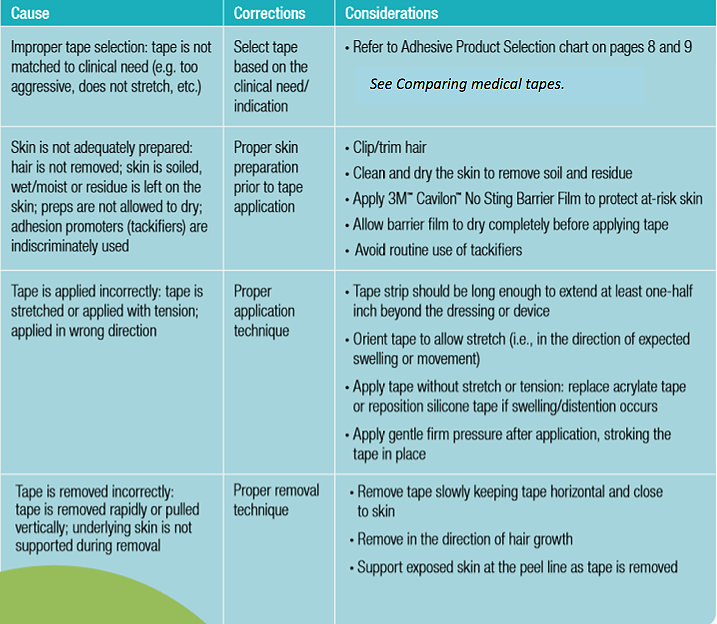 |
Evaluating MARSI risk
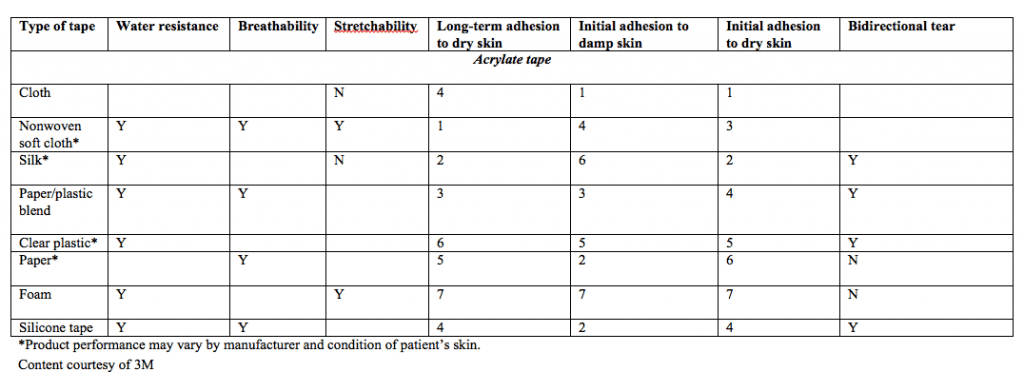
Tape should stick to the skin without causing injury. Selecting tape for a particular purpose goes beyond assessing the tape location and ambient conditions. You also must consider the patient’s underlying diagnosis and overall health. Screen for factors that increase the patient’s MARSI risk. Age can be a major risk factor.
- Neonates have thinner skin than adults. This means the epidermal layers may peel away easily during tape removal.
- Elderly patients are at risk for skin tears from moisture and loss of elasticity and strength.
Other risk factors include certain underlying diagnoses, medications, and other aspects of the patient’s current health status. Is your patient’s skin fragile or insensate? Such medications as corticosteroids can alter skin strength and elasticity, making it susceptible to tearing on tape removal. A patient with altered sensation, as from neuropathy or stroke, may not feel pain when the tape tears or strips the skin. (See the box below.)
Case studies
Your knowledge of medical tapes and the patient’s needs can help you avoid feeling overwhelmed by the large selection of tapes available—or from being surprised when a tape fails. The case studies below describe how to choose the right tape based on its purpose and location, ambient conditions, and patient assessment findings.
Mr. M
Mr. M, age 67, is hospitalized for an abdominal incision dehiscence; he has type 1 diabetes. You need to secure his abdominal dressing, which will have to be changed more than once daily because of the large amount of drainage. The goal is to protect his skin while ensuring the dressing stays in place so Mr. M can continue to get out of bed.
You determine he needs a tape that will stick to a surface that moves. Mr. M’s skin is dry but the wound produces moisture that may compromise tape adhesion. His dry skin and age put him at risk for skin tearing from loss of elasticity and moisture. Also, he’s at risk for compromised healing due to diabetes.
Considering the tape’s purpose and location and ambient conditions, you select a tape that secures the dressing without causing injury—one that’s both gentle to remove and provides sufficient adhesion to secure the dressing. For Mr. M, appropriate tape choices include both silicone and paper. Paper tape (with acrylate adhesive) is nearly as gentle as silicone. Acrylate paper tape causes trace amounts of skin stripping, while silicone tape offers greater initial and long-term adhesion than paper tape. Mr. M needs to stay mobile, so the preferred choice is silicone tape, which offers better initial adhesion. By incorporating your assessment findings and knowledge of the features of pressure-sensitive adhesives, you were able to determine which tape would best suit his needs.
J.R.
J.R., age 27, has a nasogastric (NG) tube in place for gastric decompression after removal of a perforated appendix. You note that he has oily, moist facial skin, which may cause the tape adhesive to fail, resulting in the NG tube falling out. J.R. is distressed when he learns the tube may have to be replaced if it falls out, so you decide to choose a tape that will help prevent dislodgement. The tape should be able to secure a relatively heavy tube while maintaining adhesion over time.
Considering the tape’s purpose and location and ambient conditions, you know you should pick a tape with high initial and long-term adhesion. Silk tape provides high initial adhesion to dry skin, but cloth tape offers better initial adhesion to both dry and moist skin. Washing J.R’s skin would create an ideal environment for a silk-like tape. But J.R. needs a tape that also provides adhesion over time; the moist, oily environment of his face can cause adhesive to fail. So the preferred choice for him is cloth tape, due to its increased initial adhesion on damp skin. Of course, J.R. will need ongoing evaluation to prevent tube dislodgement.
In an attempt to minimize injury, you might have chosen a gentle tape with insufficient adhesion instead of cloth tape. But tape that doesn’t secure sufficiently may allow dislodgment of critical tubing; adhesive failure occurs when tape doesn’t remain secured to the skin, tubing, or device.
As these case studies show, the condition of your patient’s skin and overall health influences tape selection. For both Mr. M and J.R., understanding the tape’s purpose and location and the ambient conditions was the launching point for tape selection. With improved knowledge of pressure-sensitive adhesives, you can evaluate tape products and select an appropriate product based on the patient’s individual needs. Your knowledge guides product selection and helps reduce the potential for injury.
Ann-Marie Taroc is a staff nurse at Seattle Children’s Hospital in Seattle, Washington, and a clinical instructor at Renton Technical College in Renton, Washington.
Selected references
3M Skin & Wound Care Division. Solutions for Securing Dressings and Devices: Because Tape Matters. 2012. http://multimedia.3m.com/mws/media/784590O/3m-medical-tapes-full-line-catalog.pdf?fn=70-2010-8488-9.pdf
Czech Z, Kowalczyk A, Swiderska J. Pressure-sensitive adhesives for medical applications. In: Akyar I, ed. Wide Spectra of Quality Control. InTech; 2011; 309-32. www.intechopen.com/books/wide-spectra-of-quality-control/pressure-sensitive-adhesives-for-medical-applications
Grove GL, Zerweck CR, Houser TP, et al. A randomized and controlled comparison of gentleness of 2 medical adhesive tapes in healthy human subjects. J Wound Ostomy Continence Nurs. 2013;40(1):51-9.
Holmes RF, Davidson MW, Thompson BJ, et al. Skin tears: care and management of the older adult at home. Home Healthc Nurse. 2013;31(2):90-101.
McNichol L, Lund C, Rosen T, et al. Medical adhesives and patient safety: state of the science: consensus statements for the assessment, prevention, and treatment of adhesive-related skin injuries. J Wound Ostomy Continence Nurs. 2013;40(4): 365-80.



















1 Comment.
My aunt is going to be getting an ostomy bag soon and she is a little worried because she has some really fragile skin. So, I was happy that you talked about how there are a lot of different types of medical tapes. It does seem like she could find on for her fragile skin. I think that she should do what you suggested about using a tape with less adhesive.