In a wide variety of settings, nurses are increasingly likely to care for patients on mechanical ventilators. Let’s assume you’re one of them. What do you need to know to plan your shift? Which patient assessment parameters are crucial? What evidence-based practice guidelines should you follow? This article discusses the top ten essentials of nursing care for ventilator patients.
Care essential 1: Review communications
Communication among care providers promotes optimal outcomes. For mechanically ventilated patients, care providers may include primary care physicians, pulmonary specialists, hospitalists, respiratory therapists, and nurses.
To make sure you’re aware of other team members’ communications about the patient, find out the goals of therapy for your patient when obtaining report. Why is she on a ventilator? To improve oxygenation? Boost ventilation? Permit sedation? Reverse respiratory muscle fatigue? Why is she on your unit? Because she has an underlying condition that complicates weaning from the ventilator? What is her do-not-resuscitate status?
Caring for patients in respiratory failure
Central lines: Recognizing, preventing, and troubleshooting complications
Understanding end-tidal CO2 monitoring
Communicating with the patient is essential, too. Provide writing tools or a communication board so she can express her needs. Ask simple yes/no questions to which she can nod or shake her head.
Care essential 2: Check ventilator settings and modes
When you enter the patient’s room, take vital signs, check oxygen saturation, listen to breath sounds, and note changes from previous findings. Also assess the patient’s pain and anxiety levels.
Read the patient’s order and obtain information about the ventilator. Compare current ventilator settings with the settings prescribed in the order. Familiarize yourself with ventilator alarms and the actions to take when an alarm sounds. Locate suction equipment and review its use. Look for a bag-valve mask, which should be available for every patient with an artificial airway; be sure you know how to hyperventilate and hyperoxygenate the patient.
Ventilator settings and modes
Generally, ventilators display ordered settings and patient parameters. Check the following settings:
- respiratory rate, the number of breaths provided by the ventilator each minute. Manually count the patient’s respiratory rate, because she may be taking her own breaths at a rate above the ventilator setting.
- fraction of inspired oxygen (FiO2), expressed as a percentage (room air is 21%).
- tidal volume (TV or VT), the volume of air inhaled with each breath, expressed in milliliters
- peak inspiratory pressure (PIP), the pressure needed to provide each breath. Target PIP is below 30 cm H2O. High PIP may indicate a kinked tube, a need for suctioning, bronchospasm, or a lung problem, such as pulmonary edema or pneumothorax.
To find out which ventilation mode or method your patient is receiving, check the ventilator itself or the respiratory flow sheet. The mode depends on patient variables, including the indication for mechanical ventilation.
Modes include those that provide specific amounts of TV during inspiration, such as assist-control (A/C) and synchronized intermittent mandatory ventilation (SIMV); and those that provide a preset level of pressure during inspiration, such as pressure support ventilation (PSV) and airway pressure release ventilation. PSV allows spontaneously breathing patients to take their own amount of TV at their own rate. A/C and continuous mandatory ventilation provide a set TV at a set respiratory rate. SIMV delivers a set volume at a set rate, but lets patients initiate their own breaths in synchrony with the ventilator.
Some patients may receive adjuvant therapy, such as positive end-expiratory pressure (PEEP). With PEEP, a small amount of continuous pressure (generally from +5 to +10 cm H2O) is added to the airway to increase therapeutic effectiveness. In many cases, PEEP is added to reduce oxygen requirements.
Finally, determine if a capnography monitor is recording the patient’s partial pressure of exhaled carbon dioxide (pCO2). Capnography, which reflects ventilation, can detect adverse respiratory events, such as tracheal-tube malpositioning, hypoventilation, and ventilator circuit problems. The capnography waveform should be square; generally, the value should be in the normal pCO2 range of 35 to 45 mm Hg. (See Normal capnography waveform) To better understand your patient’s ventilation status, check for trends in waveforms and values rather than focusing solely on single events.
Normal capnography waveform

In this normal capnography waveform, the top of the square line indicates exhaled carbon dioxide (CO2); it’s generally accompanied by a number between 35 and 45 mm Hg. The baseline should be at 0.
Care essential 3: Suction appropriately
Patients receiving positive-pressure mechanical ventilation have a tracheostomy, endotracheal, or nasotracheal tube. Most initially have an
endotracheal tube; if they stay on the ventilator for many days or weeks, a tracheotomy may be done. Tracheotomy decisions depend on patient specifics. Controversy exists as to when a tracheotomy should be considered; generally, patients have tracheotomies before being managed on a med-surg unit.
Although specific airway management guidelines exist, always check your facility’s policy and procedure manual. General suctioning recommendations include the following:
- Suction only as needed—not according to a schedule.
- Hyperoxygenate the patient before and after suctioning to help prevent oxygen desaturation.
- Don’t instill normal saline solution into the endotracheal tube in an attempt to promote secretion removal.
- Limit suctioning pressure to the lowest level needed to remove secretions.
- Suction for the shortest duration possible.
If your patient has an endotracheal tube, check for tube slippage into the right mainstem bronchus, as well as inadvertent extubation. Other complications of tracheostomy tubes include tube dislodgment, bleeding, and infection. To identify these complications, assess the tube insertion site, breath sounds, vital signs, and PIP trends. For help in assessing and managing tube complications, consult the respiratory therapist.
If your patient has a tracheostomy, perform routine cleaning and care according to facility policies and procedures.
Care essential 4: Assess pain and sedation needs
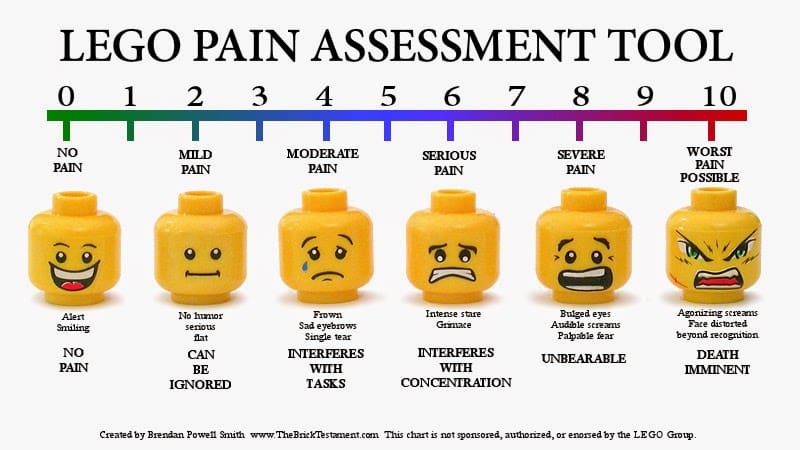
Even though your patient can’t verbally express her needs, you’ll need to assess her pain level using a reliable scale. Keep in mind that a patient’s acknowledgment of pain means pain is present and must be treated. Two scales that help you evaluate your patient’s sedation level are the Richmond Agitation Sedation Scale and the Ramsay Sedation Scale.
Should you restrain an agitated ventilator patient to prevent extubation? Research shows self-extubation can occur despite physical restraints. It’s best to treat agitation and anxiety with medication and nonpharmacologic methods, such as communication, touch, presence of family members, music, guided imagery, and distraction.
Care essential 5: Prevent infection
Ventilator-associated pneumonia (VAP) is a major complication of mechanical ventilation. Much research has focused on how best to prevent VAP. The Institute for Healthcare Improvement includes the following components in its best-practices VAP prevention “bundle”:
- Keep the head of the bed elevated 30 to 45 degrees at all times, if patient condition allows. Healthcare providers tend to overestimate bed elevation, so gauge it by looking at the bed frame rather than by simply estimating.
- Every day, provide sedation “vacations” and assess readiness to extubate, indicated by vital signs and arterial blood gas values within normal ranges as well as the patient taking breaths on her own.
- Provide peptic ulcer disease prophylaxis, as with a histamine-2 blocker such as famotidine.
- Provide deep vein thrombosis prophylaxis, as with an intermittent compression device.
- Perform oral care with chlorhexidine daily.
Other measures that decrease VAP risk include extubating the patient as quickly as possible, performing range-of-motion exercises and patient turning and positioning to prevent the effects of muscle disuse, having the patient sit up when possible to improve gas exchange, and providing appropriate nutrition to prevent a catabolic state. Assess the patient’s tolerance when she performs an activity by checking vital signs, oxygenation status, and pain and agitation levels.
Keeping bacteria out of oral secretions also reduces VAP risk. Use an endotracheal tube with a suction lumen above the endotracheal cuff to allow continuous suctioning of tracheal secretions that accumulate in the subglottic area. Don’t routinely change the ventilator circuit or tubing. Brush the patient’s teeth at least twice a day and provide oral moisturizers every 2 to 4 hours.
Care essential 6: Prevent hemodynamic instability
Monitor the patient’s blood pressure every 2 to 4 hours, especially after ventilator settings are changed or adjusted. Mechanical ventilation causes thoracic-cavity pressure to rise on inspiration, which puts pressure on blood vessels and may reduce blood flow to the heart; as a result, blood pressure may drop. To maintain hemodynamic stability, you may need to increase I.V. fluids or administer a drug such as dopamine or norepinephrine, if ordered.
High levels of inspiratory pressure with PSV and PEEP increase the risk of barotrauma and pneumothorax. To detect these complications, assess breath sounds and oxygenation status often. To help prevent these conditions, use the lowest pressure level for ventilator-delivered breaths and adjust the level as tolerated.
Care essential 7: Manage the airway
The cuff on the endotracheal or tracheostomy tube provides airway occlusion. Proper cuff inflation ensures the patient receives the proper ventilator parameters, such as TV and oxygenation. Following hospital policy, inflate the cuff and measure for proper inflation pressure using the minimal leak technique or minimal occlusive volume. These techniques help prevent tracheal irritation and damage caused by high cuff pressure; always practice them with an experienced nurse or respiratory therapist. Never add air to the cuff without using proper technique.
When performing mouth care, suction oral secretions and brush the patient’s teeth, gums, and tongue at least twice a day using
a soft pediatric or adult toothbrush. Use a tonsil suction device if your patient needs more frequent suctioning.
With assistance from an experienced colleague, change the tracheostomy tube or tracheostomy ties and endotracheal tube-securing devices if they become soiled or loose. Incorrect technique could cause accidental extubation.
Care essential 8: Meet the patient’s nutritional needs
For optimal outcomes, ventilator patients must be well nourished and should begin taking nutrition early. But like any patient who can’t swallow normally, they need an alternative nutrition route. Preferably, they should have feeding tubes with liquid nutrition provided through the gut. If this isn’t possible, the healthcare team will consider parenteral nutrition.
Patients with tracheostomy tubes may be able to swallow food. Follow the physician’s orders and consult speech and respiratory therapists.
Care essential 9: Wean the patient from the ventilator appropriately
As your patient’s indications for mechanical ventilation resolve and she’s able to take more breaths on her own, the healthcare team will consider removing her from the ventilator. Weaning methods may vary by facility and provider preference. Although protocols may be used to guide ventilator withdrawal, the best methods involve teamwork, consistent evaluation of patient parameters, and adjustment based on these changes.
Some patients may need weeks of gradually reduced ventilator assistance before they can be extubated; others can’t be weaned at all. Factors that affect ease of weaning include underlying disease processes, such as chronic obstructive pulmonary disease or peripheral vascular disease; medications used to treat anxiety and pain; and nutritional status.
Care essential 10: Educate the patient and family
Seeing a loved one attached to a mechanical ventilator is frightening. To ease distress in the patient and family, teach them why mechanical ventilation is needed and emphasize the positive outcomes it can provide. Each time you enter the patient’s room, explain what you’re doing. Reinforce the need and reason for multiple assessments and procedures, such as laboratory tests and X-rays. Communicate desired outcomes and progression toward outcomes so the patient and family can actively participate in the plan of care.
Caring for a patient on mechanical ventilation requires teamwork, knowledge of care goals, and interventions based on best practices, patient needs, and response to therapy. Mechanical ventilation has become a common treatment, and nurses must be knowledgeable and confident when caring for ventilator patients.
American Association of Critical-Care Nurses. AACN Practice Alert: Oral care for patients at
risk for ventilator-associated pneumonia; 2010.
www.aacn.org/WD/Practice/Docs/PracticeAlerts/oral%20care%2004-2010%20final.pdf.
Accessed February 19, 2012.
American Association of Critical-Care Nurses. AACN Practice Alert: Ventilator Associated
Pneumonia; 2008.
www.aacn.org/WD/Practice/Docs/PracticeAlerts/Ventilator_Associated_Pneumonia_1-2008.pdf.
Accessed January 17, 2012.
American Association for Respiratory Care. AARC Clinical Practice Guidelines. Endotracheal
suctioning of mechanically ventilated patients with artificial airways. Respir Care. 2010
June;55(6):758-64.
Bailey P, Thomsen GE, Spuhler VJ, et al. Early activity is feasible and safe in respiratory failure
patients. Crit Care Med. 2007 Jan;35(1):139-45.
Blackwood B, Alderdice F, Burns KE, Cardwell CR, Lavery GG, O’Halloran P. Protocolized vs.
non-protocolized weaning for reducing the duration of mechanical ventilation in critically ill adult patients: Cochrane Review Protocol. J Adv Nurs. 2009 May;65(5):957-64.
Burns SM. Pressure modes of mechanical ventilation: the good, the bad, and the ugly. AACN
Adv Crit Care. 2008 Oct-Dec;19(4):399-411.
Campbell ML. How to withdraw mechanical ventilation: a systematic review of the literature.
AACN Adv Crit Care. 2007 Oct-Dec;18(4):397-403.
Chang LY, Wang KW, Chao YF. Influence of physical restraint on unplanned extubation of adult
intensive care patients: a case-control study. Am J Crit Care. 2008 Sep;17(5):408-15.
Coffin SE, Klompas M, Classen D, et al. Strategies to prevent ventilator-associated pneumonia in
acute care hospitals. Infect Control Hosp Epidemiol. 2008 Oct;29 Suppl 1:S31-40.
Institute for Healthcare Improvement. Implement the IHI Ventilator Bundle. 2011.
www.ihi.org/knowledge/Pages/Changes/ImplementtheVentilatorBundle.aspx. Accessed January
17, 2012.
Kjonegaard R, Fields W, King ML. Current practice in airway management: a descriptive
evaluation. Am J Crit Care. 2010 Mar;19(2):168-73.
Lyerla F, LeRouge C, Cooke DA, Turpin D, Wilson L. A nursing clinical decision support system
and potential predictors of head-of-bed position for patients receiving mechanical ventilation. Am J Crit Care. 2010 Jan;10(1):39-47.
Pun BT, Dunn J. The sedation of critically ill adults; part 2: management. July 2007. Am J Nurs.
2007 Aug;107(8):40-9.
Rassin N, Sruyah R, Kahalon A, Naveh R, Nicar I, Silner D. “Between the fixed and the
changing”: examining and comparing reliability and validity of 3 sedation-agitation measurement scales. Dimens Crit Care Nurs. 2007 Mar-Apr;26(2):76-82.
Worrall CL, Anger BP, Simpson KN, Leon SM. Impact of hospital-acquired/ventilator-associated/healthcare-associated pneumonia practice guideline on outcomes in surgical trauma patients. J Trauma. 2010 Feb;68(2):382-6.
Laura C. Parker is an assistant professor of nursing at the County College of Morris in Randolph, New Jersey.



















26 Comments.
i have really learned a lot since i have been managing patients on mechanical ventilation with covid-19 associated with pneumonitis
thank you so much for this article. it was very helpful.
Where could I find actual published clinical practice guidelines for communicating with patients on mechanical ventilation?
THANKS FOR THE INFORMATION.THIS IS VERY USE FULL TO ME
Simple and effective
Is it advisable to put femur bone surgical patient in ventilator? There is any other alternative way to treat this patient without put into in ventilator? If it has been detected that patient effected by VAP pneumonia then doctor should keep patient in ventilator support or not?
thank so much
ITS GUD …….
thank you so much for this article. it was very helpful.
Hi,
I just want to ask ur expert on nursing part while pt has been oder by a doctor for chest physiotherapy. In that case the pt was on ventilation machine support, while the physio do her jobs what does the nurse do? Please answer me ASAP.
nice review
thanks for the information, valuable information
Thanks for a simple review.
simple and valuable
thanks
Thank you for this very easy refresher !
quite useful review……
A wealth of information, thanks a tone.
thanks 4 these tips
THANKS FOR THIS ARTICLE ITS VERY IMPORTEND NOTS. SO THANKS
Thanks for this article,Its very useful and eassy to understand nurses.And we can provide good care for such a patients
very useful… thank u sooo much
thanks for the article. this is very helpful and very refreshing since it has been a while since I have cared for a ventilator patient
may i get a questionnaire t o assess the level of the satisfation in communication of mechanically ventilated patients?????
Great If I learn and understand these 10 steps like the alphabet, then I will be able to confidently provide safe and efficient quality care to my home care patients – LPN studying for RN license.
Lesley I gues this because nurses look at the whole patient and RRT often only assess respiratory status. In most cases the RRT will perform the task of operating the ventilator and assist to maintain the patient’s airway, but ultimately the nurse is the primary caregiver.
I would like to note that the professional licensed practice of Respiratory Care (e.g. Respiratory Therapists) is noted only once in this whole article. Having been in the field and worked shoulder to shoulder with CCRNs for over 30 years I find this very very sad. I appreciate that nurses (as the primary care givers) want to be as knowledgeable about their patients as possible, but why is there no suggestion to ask the expert users about the best care for their ventilator patient?