Research can be conducted using either quantitative or qualitative methods. The distinction is crucial. Perhaps because of today’s emphasis on numerical data in health care, most nursing research is quantitative. Although quantitative studies yield valuable information that contributes to practice change, their predominance sometimes can obscure the valuable contribution qualitative research can make in generating new knowledge and ultimately influencing the practice of nursing and other health professions.
In recent years, many healthcare organizations have shifted their focus to a patient-centered model in which patients are involved in decision-making and their preferences are honored. This model has been reinforced by regulators who focus on the patient experience and achieving favorable patient outcomes; in some cases, these outcomes are tied to reimbursement. The only way to obtain information about patients’ (and families’) perspectives is to ask them, to listen and learn from them, and to incorporate their responses into the delivery of care. Qualitative research does just that.
Observation and interview
Qualitative researchers use the research process to conduct a systematic investigation into patient and family perspectives and make recommendations based on their responses that can advance the patient-centered model. Essentially, the goal of qualitative research is to understand a particular phenomenon from the viewpoint of those who’ve experienced it. In other words, the researcher is open to learning from people with firsthand experience of an event, a situation, or a set of circumstances.
Observation and interview are the main methods used to obtain such data (although sometimes artwork, journals, photos, and documents are used to further elicit understanding). The researcher analyzes the data, searching for patterns, regularities, and commonalties shared by most or all participants. The result is a number of themes, or dimensions, of the phenomenon that together yield deeper insight into that phenomenon and participants’ experience of it.
An aid to treatment planning and approach to care
Findings from qualitative studies can guide healthcare providers in planning treatment and approaches to patient care that meet patients’ needs. For example, many patients with end-stage heart failure (HF) or chronic obstructive pulmonary disease (COPD) die in hospitals during an acute event without expressing their choices or preparing for the end of life. Lowey et al. (2013) undertook a qualitative study to understand the experiences and goals of home healthcare patients with end-stage HF or COPD. They conducted 40 interviews with 20 participants who had either advanced HF or COPD and were treated in one of two home healthcare agencies. Interview findings indicated participants identified severe shortness of breath as engulfing “everything in life” and limiting their daily activities—yet they didn’t associate these symptoms with being near the end of their lives. The patients didn’t want to report these symptoms because they didn’t want to be hospitalized. Their goals
for care were shaped by previous experiences of recovering from exacerbations. They were sure that if their illness were life-threatening, their healthcare provider would communicate this to them clearly. Furthermore, while they knew their illness wouldn’t improve, they hoped it would remain stable—and maintained that hope while living with worsening symptoms.
Based on these results, the researchers made the following recommendations to clinicians:
- Improve communication with patients about their prognosis so they can make appropriate, informed decisions about their care.
- Examine their transition-of-care practices.
- Place such patients with a homecare team that provides palliative care for better symptom management.
The researchers also urged healthcare professionals to expedite implementation of these recommendations to ease patient suffering.
Informing policy and protocol development
Findings from qualitative studies can be used to inform policy and protocol development. For example, Aburn and Gott (2014) sought to understand the perceptions and experiences of parents and caregivers of children newly diagnosed with acute lymphoblastic leukemia. They were particularly interested in their experiences of the education they received about their child’s diagnosis and the care required at home. The researchers recognized that with the increasing shift of care to the home rather than the hospital, it’s important to assess how parents and caregivers are educated so they can provide safe, effective care to their children.
Themes that emerged from the researchers’ audiotaped interviews with 12 parents or other home caregivers revealed that they:
- couldn’t absorb all the information they were given initially, due to the immense stress they were experiencing
- appreciated getting information and education from the same nurse, believing such continuity benefited them and their child
- valued frequent conversations with healthcare providers as a way of learning
- found the written information they received used too much medical terminology and was out of date or irrelevant to their needs
- found the websites provided to them were outdated. Most parents had done their own Internet searches but found the results too grim or inaccurate.
Study findings were reported to the policymakers and clinicians on the unit to inform policy and protocol changes. A particular recommendation was standardizing education given by all nursing staff. It was expected that implementing changes in education practices would help parents and other caregivers feel more confident in the care they provide to their children.
Qualitative research on bedside nursing handover
In another study, Jeffs et al. (2014) sought to understand patients’ experiences of the recently implemented process of bedside nursing handover. While it has been widely accepted that bedside nursing handover helps ensure patient safety and quality care, the researchers believed it was important to know how patients view this process. They interviewed 45 participants from various clinical areas in a large academic medical center. They asked open-ended questions about their experiences, how the process benefited them, the challenges they encountered, and any recommendations for improvement.
Themes that emerged from these interviews revealed that the most common positive comments concerned introduction of the incoming nurse. Participants saw the introduction as a personal touch that gave them a sense of security and comfort. They felt more confident in their care because the incoming nurse had a better understanding of how to plan and carry out their care. Participants also viewed bedside nursing handover as an opportunity for them to ask questions, give input into their care, correct inaccurate information, and identify missed care. Some reported that the interaction also relieved anxiety and fear. However, variation existed in the degree to which patients wanted to be engaged in their care and the amount and type of information they wanted to discuss. While most patients chose to participate in bedside nursing handover, some didn’t; they found the process redundant (particularly if their stay was long-term) or weren’t comfortable with the exchange taking place at the bedside.
The researchers noted that although their findings indicated most patients perceived bedside nursing handover as beneficial, the results also showed the importance of being sensitive to and honoring patient choices about the level of involvement with which they were comfortable and their preference for the type of bedside interaction. Therefore, nurses need to be knowledgeable about patients’ choices and show flexibility in supporting them.
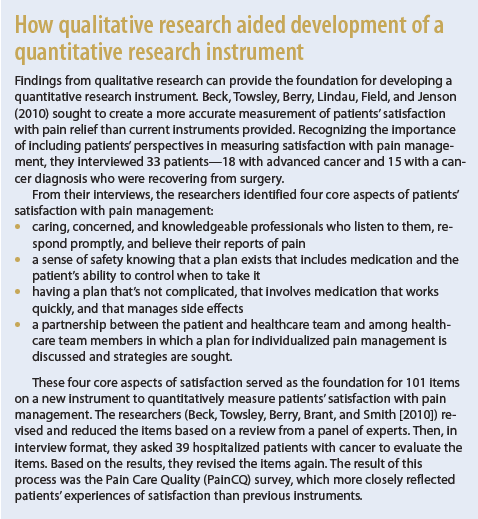
As our examples show, qualitative methods capture patients’ perspectives and add a dimension to our knowledge that quantitative methods alone can’t obtain. (See How qualitative research aided development of a quantitative research instrument.) Qualitative and quantitative methods complement each other, giving us the best of both worlds when we base our practice on the results of both methods.
Selected references
Aburn G, Gott M. Education given to parents of children newly diagnosed with acute lymphoblastic leukemia: the parent’s perspective. Pediatr Nurs. 2014;40(5):243-8, 256.
Beck SL, Towsley GL, Berry PH, Lindau K, Field RB, Jenson S. Core aspects of satisfaction with pain management: cancer patients’ perspectives. J Pain Symptom Manage. 2010;39(1):100-5.
Beck SL, Towsley GL, Berry PH, Brant JM, Smith EM. Measuring the quality of care related to pain management: a multiple-method approach to instrument development. Nurs Res. 2010;59(2):85-92.
Hedges C, Williams B. Anatomy of Research for Nurses. Indianapolis, IN: Sigma Theta Tau International; 2014.
Jeffs L, Beswick S, Acott A, et al. Patients’ views on bedside nursing handover: creating a space to connect. J Nurs Care Qual. 2014; 29(2):149-54.
Lowey SE, Norton SA, Quinn JR, Quill TE. Living with advanced heart failure or COPD: experiences and goals of individuals nearing the end of life. Res Nurs Health. 2013;36(4):349-58.
Barbara Williams is a nurse scientist at Meridian Health in the Ann May Center for Nursing and Allied Health in Neptune, New Jersey; an instructor in the nursing program at William Patterson University in Wayne, New Jersey; and coauthor of Anatomy of Research for Nurses.



















1 Comment.
Wonder resources on nursing research models.