Nasogastric (NG) tubes are placed to administer enteral nutrition, medications, or fluids to children of all ages who are unable to ingest enough proper nutrition by mouth to grow and develop normally. Most NG tubes are placed at the bedside. As innocuous as the insertion procedure might seem, it carries a risk of serious or even potentially lethal complications.
Abdominal X-ray is the gold standard for verifying that an NG tube is placed correctly in the stomach (and not the esophagus, small bowel, or lung), but this method involves repeated radiation exposure and isn’t widely used in pediatrics. Typical bedside methods for confirming correct placement include auscultation of air insufflated over the abdomen, gastric secretion pH measurement, visual inspection of aspirated gastric secretions, capnography, age-related height-based measurement, and use of an electromagnetic device (such as the CORTRAK® 2 Enteral Access System).
No universal standard of practice exists for bedside verification because each method has limitations.
- Auscultation: This technique can detect sounds in the epigastrium regardless of tube location, so a tube misplaced in the lung may transmit sounds audible in the stomach.
- Gastric pH measurement: Acid-suppressing drugs or enteral formula in the stomach may raise pH above the accepted cutoff level of 5, which typically indicates the tube is in the stomach.
- Aspiration of gastric contents: Obtaining aspirate can be difficult with the small-bore feeding tubes used in pediatric patients. Also, pulmonary or small-bowel secretions may be hard to distinguish from gastric secretions.
- Capnography: While this technique can determine if the NG tube is in the lungs via carbon dioxide detection, it doesn’t ensure the tube is in the stomach.
- Age-related height-based measurement: Using this equation helps predict initial tube placement length but not tube location.
- Electromagnetic device: This method can be used only in larger children who can tolerate an 8 Fr diameter tube. It’s rarely used in pediatric practice.
Reports of inadvertent NG tube placement in the lung prompted safety alerts from the Health Service in the United Kingdom and the Child Health Patient Safety Organization (CHPSO) in the United States. CHPSO’s 2012 alert called for immediate discontinuation of auscultation as a verification method and recommended gastric pH measurement as the most evidence-based method.
NOVEL response
In response to alerts and concerns about lack of reliable methods to verify tube placement, the American Society for Parenteral and Enteral Nutrition established the New Opportunities for Verification of Enteral Tube Location (NOVEL) Project. (Note: The authors are members of the NOVEL Project.) Participating organizations include the American Association of Critical-Care Nurses, Society of Pediatric Nurses, American Association for the Advancement of Medical Instrumentation, National Association of Neonatal Nurses, and CHPSO. Other NOVEL members include biomedical engineers and a parent who lost her son due to a misplaced NG tube. NOVEL seeks to disseminate best-practice information to staff nurses to promote consistency and improve care at the bedside.
NOVEL’s initial mission was to work with inventors and industry to “develop or morph existing technologies to allow for nonradiologic verification of feeding tube placement.” Several prototypes are in the pipeline. When it became apparent that the technology for bedside use wouldn’t be available for years, NOVEL expanded its mission to include research to determine best practices in three target pediatric populations—neonates, pediatric inpatients, and pediatric home care patients.
In January 2015, NOVEL completed a 1-day point prevalence study to determine how often NG tubes are used in hospitalized pediatric patients and how participating organizations verify tube placement. In the 63 hospitals that participated in this study, 24% of patients admitted on data-collection day had feeding tubes; of these patients, 66% had NG tubes, 21% had orogastric tubes, and 17% had postpyloric tubes. Most of these patients (61%) were in neonatal intensive care units (NICUs); 21%, in medical-surgical units, and 17%, in pediatric intensive care units. Patients’ average age was 14 months, but the median age and mode age were both 1 month, indicating they were mostly infants. Average weight was 6.8 kg (15 lb); mode weight was 2.2 kg (4.8 lb), and median weight was 2.8 kg (6.2 lb), indicating they were small infants. The most commonly used feeding tube size was 5 Fr, reflecting the common use of small-diameter tubes in small infants. Tube size ranged from 5 to 8 Fr.
We asked participating hospitals to rank the most common methods they used to verify tube placement. Aspiration and auscultation ranked number 1 and 2 overall. Only 10 hospitals listed pH measurement as the preferred method. By hospital type, primary verification methods were as follows:
- pediatric hospitals: aspiration of gastric contents, abdominal X-ray, and measurement of external tube length before placement
- adult hospitals with NICUs: auscultation and aspiration of gastric contents
- adult hospitals with pediatric and NICU populations: aspiration, auscultation, and abdominal X-ray.
NOVEL Project members recognize lack of consistency in how nurses verify NG tube placement. We also acknowledge the need for staff nurses to use their best judgment when inserting NG tubes in patients who have an increased work of breathing or a neurologic impairment with a weak or absent gag reflex, as well as those who are unable to aspirate anything from the feeding tube and those who’ve suffered respiratory arrest. In these situations, experts recommend verifying tube placement with an abdominal X-ray, because any bedside method (even gastric pH measurement) could be inaccurate or misleading.
Ensuring correct NG tube placement
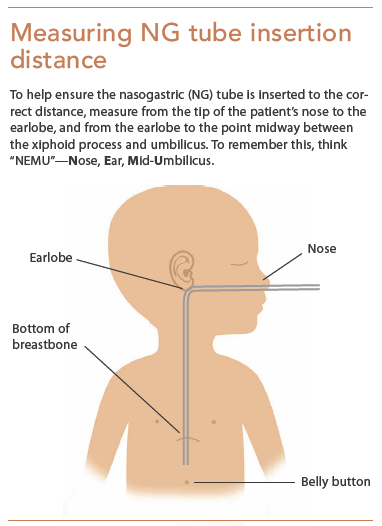
Be sure to use the correct method for determining if the NG tube is inserted to the correct distance. (See Measuring NG tube insertion distance.) Carefully document the procedure and method you used to verify tube placement.
Also review your hospital’s procedure for verifying NG tube placement. If it recommends auscultation and aspiration, organize a group to review the literature and discuss gastric pH measurement instead. A combination of methods may be acceptable for verifying placement, but make sure evidence exists to guide your practice. In addition, consider whether your hospital might benefit from an enteral access team (much like a vascular access team). Taking these steps can improve safety for pediatric patients with NG tubes. If you’re unsure whether a patient’s NG tube is correctly placed, ask for an abdominal X-ray to confirm placement.
The authors are members of the NOVEL Project. Beth Lyman is senior program director for the nutrition support team at Children’s Mercy, Kansas City in Kansas City, Missouri, and chair of the NOVEL Project. Jane Anne Yaworksi is a clinical nurse specialist in nutrition support and intestinal care at Children’s Hospital of Pittsburgh in Pittsburgh, Pennsylvania. Lori Duesing is a pediatric nurse practitioner in the acute care division of gastroenterology and nutrition at Children’s Hospital of Wisconsin in Milwaukee. Candice Moore is a nurse in the gastroenterology department at Cincinnati Children’s Hospital in Cincinnati, Ohio.
Selected references
Beckstrand J, Cirgin Ellett ML, McDaniel A. Predicting internal distance to the stomach for positioning nasogastric and orogastric feeding tubes in children. J Adv Nurs. 2007;59(3):274-89.
Child Health Patient Safety Organization; ECRI Institute. Patient Safety Action Alert. Event: Blind Pediatric NG Tube Placements – Continue to Cause Harm. August 2012. https://goo.gl/8y1o6J
Ellett ML, Croffie JM, Cohen MD, Perkins SM. Gastric tube placement in young children. Clin Nurs Res. 2005;14(3):238-52.
Gilbertson HR, Rogers EJ, Ukoumunne OC. Determination of a practical pH cutoff level for reliable confirmation of nasogastric tube placement. JPEN J Parenter Enteral Nutr. 2011;35(4):540-4.
Irving SY, Lyman B, Northington L, et al; NOVEL Project Work Group. Nasogastric tube placement and verification in children: review of the current literature. Crit Care Nurs. 2014;34(3):67-78.
Kleinerman RA. Cancer risks following diagnostic and therapeutic
radiation exposure in children. Pediatr Radiol. 2006;36 Suppl 2:121-5.
Lyman B, Kemper C, Northington L, et al. Use of temporary enteral access devices in hospitalized neonatal and pediatric patients in the United States. JPEN J Parenter Enteral Nutr. 2015;1-7
National Health Service. Patient Safety Alert. Placement devices for nasogastric tube insertion do not replace initial position checks. December 2013. england.nhs.uk/wp-content/uploads/2013/12/psa-ng-tube.pdf
Renner M. Far from reliable: pH testing in the neonatal intensive care unit. J Pediatr Nurs. 2010;25(6):580-3.
Westhus N. Methods to test feeding tube placement in children. MCN Am J Matern Child Nurs. 2004;29(5):282-7.



















1 Comment.
I just wanted to comment on Small Bore Feeding Tube placement using the Cortrak system in pediatric patients. Our placement team utilizes the 8fr tube routinely in small children. All placements are considered on an individual basis and collaborative events with input from the primary nurse, primary care staff and the child’s parents.
As suggested the first step to safe placement is to question whether the tube should be placed at all.