Safe, effective pain control hinges on a multimodal approach that addresses the cause of pain and uses medications and other interventions that relieve the patient’s specific type of pain. With the multimodal approach, individual medications and interventions are chosen for their action on different parts of the pain pathway. This reduces the required dosages of each analgesic, reducing side effects while improving pain relief.
First-line analgesics can be classified in several different ways. One classification system focuses on the type of pain present—acute, postoperative, chronic, cancer, or neuropathic.
Using a different classification system, the World Health Organization (WHO) grouped analgesics into four categories and developed an analgesic ladder for cancer pain management. The ladder provides a stepwise method to guide pain management in cancer patients experiencing pain ranging from mild to severe. This stepwise approach also may apply to treatment of other types of pain. More recently, it was adapted to guide pain management in postprocedural patients. (See the box below.)
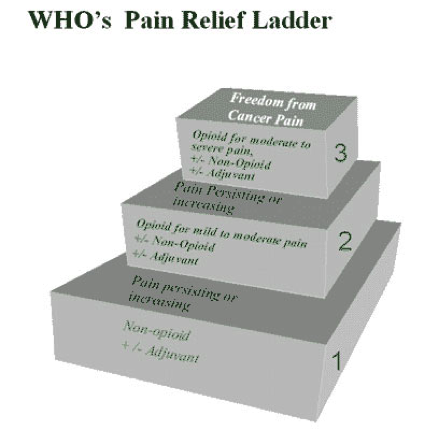 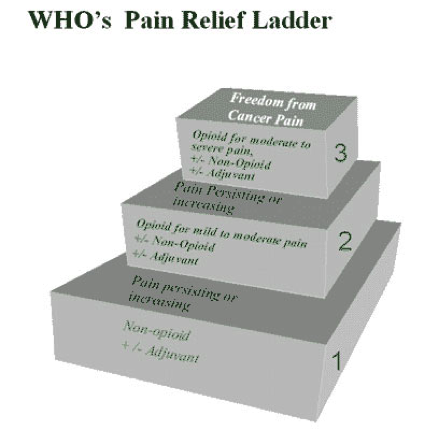 |
The WHO ladder provides a logical framework for categorizing first-line analgesics into three groups:
- nonopioids—acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs)
- adjuvant analgesics—local anesthetics, anticonvulsants, and antidepressants
- opioids. (See the box below.)
WHO analgesic categoriesThe table below shows specific medications in each of the World Health Organization’s analgesic categories.
|
Step 1 of the WHO analgesic ladder consists of a nonopioid, given with or without adjuvants depending on the type of pain. Step 2 includes step-1 agents plus an opioid for mild to moderate pain. Step 3 consists of step-2 agents plus one or more single-entity opioids for moderate to severe pain.
Ladder step 1: Nonopioids and/or adjuvants for mild to moderate pain
Acetaminophen, an over-the-counter (OTC) analgesic, typically is the first medication used for mild to moderate pain. However, because it’s metabolized in the liver, its use is limited by a dose ceiling. In 2014, the Food and Drug Administration (FDA) set the total limit for acetaminophen at 4,000 mg/day for adults. The agency cautioned that because many medications are available in combination with acetaminophen, the risk of accidentally taking too much acetaminophen exists. Therefore, the acetaminophen dosage in combination products shouldn’t exceed 325 mg.
- Safe dosing: 650 mg every 4 hours; may be increased to 1,000 mg four times daily
- Monitor liver function. Ask the patient about alcohol consumption. Teach adults not to exceed 4,000 mg/day from all sources (unless a healthcare provider instructs them to limit the daily total dosage to less than 4,000 mg). Caution patients not to use acetaminophen if they have liver disease or when drinking alcoholic beverages.
Nonselective nonsteroidal anti-inflammatory drugs (NSAIDs). Available in several formulations, these drugs are effective for mild to moderate pain. NSAID has unique dosing recommendations and cautions. Nonselective NSAIDs can cause dose-related side effects, including gastric irritation and platelet inhibition. They are contraindicated in various medical conditions and rarely should be used in older adults. NSAIDs are available in both OTC and prescription strengths and can be given by various routes.
- Safe dosing: varies; see guidelines for the specific NSAID. Generally, start with a low dosage and titrate upward to a safe, effective dosage.
- Monitor for contraindications specific to the NSAID. Stay alert for exacerbation of diagnosed hypertension and cardiovascular disease.
- Teach¬ patients to start with the lowest possible dosage. Tell them to never take more than one NSAID at a time. Review precautions for the specific NSAID they’re using and patient comorbidities.
Selective NSAIDs. Celecoxib, the only COX-2 selective NSAID available in the United States, isn’t recommended for patients with cardiovascular disease, hypertension, renal insufficiency, or sulfur allergy. It’s less likely to cause GI adverse side effects than non-selective NSAIDS.
- Safe dosing: 200 mg twice daily
- Monitor for contraindications, such as cardiovascular disease and sulfonamide allergy.
- Teach patients not to take celecoxib with other prescription or OTC NSAIDs.
Adjuvants
Local anesthetics include the lidocaine patch 5% and lidocaine gel 5%. Generally considered safe, local anesthetics relieve pain in a localized area. Indications include postherpetic neuralgia and neuropathic pain limited to a specific location.
- Safe dosing: up to three patches applied for 12 consecutive hours, then removed and not replaced for another 12 hours
- Monitor for skin irritation and blanching at the application site. Discontinue use if these develop.
- Teach patients they may cut patches to fit the affected area. Advise them to report blanching or skin irritation and remove the patch if these side effects occur.
Tricyclic antidepressants (including desipramine, nortriptyline, and amitriptyline) are considered first-line drugs for treating neuropathic pain by the International Association for the Study of Pain. Use amitriptyline only if desipramine and nortriptyline aren’t available.
- Safe dosing: varies with the particular drug and the patient’s age and comorbidities. Preferably, start with a low dosage and titrate upward slowly over several weeks.
- Monitor for anticholinergic and other drug-specific adverse effects.
- Teach patients that desired effects may take several days to occur. Advise them to report adverse effects, such as sedation or dizziness.
Serotonin-norepinephrine reuptake inhibitors (SSRIs), particularly duloxetine and venlafaxine, are effective first-line medications for neuropathic pain.
- Safe dosing: For duloxetine, start with 20 mg/day and titrate as needed up to 60 mg/day, not to exceed 120 mg/day. For venlafaxine, start with 37.5 mg/day and increase if needed to 150 to 225 mg/day. For both medications, titrate to analgesic effectiveness over several weeks.
- Monitor blood pressure and stay alert for drug-specific adverse effects. When discontinuing venlafaxine, taper the dosage to prevent withdrawal symptoms.
- Teach patients to report adverse effects. Tell them how long it may take for the drug to produce effective pain control. Advise them not to stop taking the drug abruptly.
Gabapentinoid anticonvulsants commonly are used to treat neuropathic pain. Gabapentin and pregabalin are calcium-channel ligands recommended as first-line drugs for neuropathic pain.
- Safe dosing: varies with the particular drug and the patient’s age and comorbidities. Generally, start with a low dosage and titrate upward slowly to a dosage that produces safe, effective pain control. Gabapentin commonly is started at 300 mg three times daily; however, in older adults, start with 100 mg at the hour of sleep. It can be titrated up to a total daily dose of 3,600 mg in patients who tolerate it. Pregabalin commonly is started at 50 mg three times daily or 75 mg twice daily; it can be titrated to a total daily dose of 600 mg.
- Monitor for somnolence, dizziness, fatigue, and ataxia. Check laboratory results for renal impairment, such as elevated plasma drug concentration and prolonged drug elimination.
- Teach patients to report adverse effects or unusual symptoms. Inform them the dosage may need to be increased gradually before the drug can control pain effectively.
Ladder step 2: Opioids for mild to moderate pain
In step 2, oral opioid analgesics for mild to moderate pain are added to the analgesic plan of care when nonopioids and adjuvants don’t provide effective pain relief.
Hydrocodone commonly is prescribed for moderate to severe pain. It’s available in combination with other analgesics (such as acetaminophen, aspirin, or ibuprofen). While the combination of hydrocodone and a nonopioid can yield greater effectiveness, the dosage is limited by the nonopioid component, which also limits the hydrocodone dosage.
- Safe dosing: 5 to 10 mg every 4 or 6 hours
- Monitor for drug allergies or comorbidities that may limit the acetaminophen, aspirin, or ibuprofen dosage. Maximum acetaminophen dosage is 4 g/day; maximum aspirin and ibuprofen dosages are specific to the patient and medication.
- Teach patients taking a combination product to include the acetaminophen dosage when calculating the total daily amount of acetaminophen they’re taking. Tell them the total shouldn’t exceed 4 g/day (or a lower limit if directed by their primary care provider).
Tramadol, an atypical opioid, is a dual-mechanism analgesic. It functions as an agonist at mu opioid-receptor sites and inhibits monoamine reuptake, thus blocking serotonin and norepinephrine reuptake. Tramadol is effective for pain associated with arthritis, back pain, and neuropathy. The dosage may be increased slowly over several weeks; the drug should be withdrawn gradually. Don’t give tramadol to patients with a history of seizures.
- Safe dosing: 50 to 100 mg every 3 to 7 hours. Maximum total daily dosage shouldn’t exceed 300 mg in adults older than age 75 or 400 mg in younger adults.
- Monitor for history or current use of SSRIs, which may increase the risk of serotonin syndrome. This potentially life-threatening condition is characterized by mental status changes, dysautonomia, and neuromuscular dysfunction (separately or in combination).
- Teach patients to report dizziness, somnolence, nausea, and other adverse effects. Caution them not to discontinue the drug abruptly. Inform those with pain-management agreements or contracts and those in substance-abuse treatment programs that tramadol is an opioid.
Oxycodone, an oral opioid, commonly is prescribed in an immediate-release form that includes acetaminophen or aspirin. In this combination form, oxycodone is used for moderate pain because the ceiling dosage of acetaminophen or aspirin limits the oxycodone dosage.
- Safe dosing: limited by the safe daily dosage of the nonopioid component
- Monitor for allergies. Check the patient’s history for comorbidities that may limit the amount of acetaminophen, aspirin, or ibuprofen the patient can take.
- Teach patients taking an oxycodone-acetaminophen combination product to include the acetaminophen dosage in the total daily acetaminophen amount. Caution them not to exceed 4 g/day of acetaminophen (or a lower limit if directed by their primary care provider).
Ladder step 3: Single-entity opioids for moderate to severe pain
Single-entity opioids include morphine, oxycodone, fentanyl, and hydromorphone. These come in forms that can be administered by various routes. The least invasive route is recommended. (See the box below.)
Common single-entity opioidsMorphine, considered the gold standard of opioids, is available for oral, rectal, I.V., subcutaneous, intrathecal, epidural, or intranasal administration. Oral morphine comes in tablets and an elixir in immediate-release (IR) and extended-release (ER) products. Since ER morphine is available in both 12-and 24-hour products, be sure to clarify the dosing frequency for the particular medication prescribed. Confusing the dosages of the 12-hour and 24 hour products can result in under- or over-dosing. Oxycodone, an oral opioid, is available in tablets and elixir form, in both IR and ER products. IR oxycodone in a single-entity product is indicated for moderate to severe pain. Teach patients the difference in dosages between the IR and ER formulations. Caution them never to cut or chew the ER product. Fentanyl, a synthetic opioid, comes in forms that are given by the I.V., subcutaneous, transdermal, or transmucosal route. It’s approximately 100 times more potent than morphine. Pay close attention to safe dosing guidelines. Keep in mind that fentanyl is prescribed in micrograms (mcg), not milligrams (mg). Transdermal fentanyl (not indicated for acute pain or for opioid-naïve patients) can be helpful in patients with swallowing or GI problems. Each transdermal patch delivers the prescribed amount of drug over a 72-hour period. Because fentanyl is lipophilic, patients using a fentanyl patch must have adequate body fat to absorb the drug adequately. Teach patients to apply the patch over an area with adequate subcutaneous tissue. Caution them never to cut or apply heat over the patches, and to keep them out of the reach of children and pets while they’re wearing or storing the patch. Hydromorphone, a semisynthetic opioid, comes in forms that can be given by the oral, subcutaneous, I.V., intrathecal, or epidural route. Its equianalgesic dosage ranges from 1:4 to 1:11. This means a 1-mg dose of hydromorphone is comparable to a morphine dosage between 4 and 11 mg. The estimated relative potency of hydromorphone to morphine is 7.5:1. The reason for the wide range isn’t clear but may stem in part from individual patient characteristics. |
- Safe dosing: individualized; determined by the amount of opioid needed to safely control pain, but limited by the need to minimize adverse effects.
- Monitor for contraindications, allergies, and concomitant use of other medications with a synergistic effect (causing or increasing sedation). Assess the patient for adverse effects, including sedation, impaired respiratory status, nausea, pruritus, and constipation.
- Teach patients about the goals of opioid therapy. Carefully review dosing instructions. Caution them not to cut or crush ER products. To help prevent constipation, instruct them to follow a bowel regimen that promotes regular bowel evacuation.
Analgesic pearls
Keep the following points in mind to help maximize your patient’s pain relief regimen:
- Use what has worked before to control the patient’s pain. If a particular drug wasn’t effective in the past, it probably won’t be effective now.
- When moving a patient from one step of the analgesic ladder to the next, continue drugs from the previous steps—unless the patient has experienced adverse effects, the added medication duplicates the action of another one the patient’s taking, or the drug is contraindicated for the patient.
- Start at a low dosage and increase the dosage slowly, especially in older adults.
- Use the lowest effective dosage, and only when necessary. However, giving a dose to prevent pain before an activity that’s known to cause pain (such as wound care or physical therapy) is acceptable.
- Remember—sedation always precedes respiratory depression.
- Assess the patient for pain control and safety, including sedation and respiratory status.
- Know that if the patient can’t afford a medication, he or she won’t adhere to its use.
Selected references
Arnstein P. Clinical Coach for Effective Pain Management. Philadelphia, PA: F.A. Davis: 2010.
Barkin RL, Beckerman M, Blum SL, et al. Should nonsteroidal anti-inflammatory drugs (NSAIDs) be prescribed to the older adult? Drugs Aging. 2010;27(10):775-89.
Crews JC. Multimodal pain management strategies for office-based and ambulatory procedures. JAMA. 2008;288(5):629-32.
D’Arcy Y. Compact Clinical Guide to Chronic Pain Management. New York, NY: Springer Publishing Co.; 2011.
Duke AN, Bigelow GE, Lanier RK, et al. Discriminative stimulus effects of tramadol in humans. J Pharmacol Exp Ther. 2011;338(1):255-62.
Dworkin RH, O’Connor AB, Audette J, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc. 2010;85(3 Suppl):S3-S14.
Evans RW, Tepper SJ, Shapiro, RE, et al. The FDA alert on serotonin syndrome with use of triptans combined with selective serotonin reuptake inhibitors or selective serotonin-norepinephrine reuptake inhibitors: American Headache Society position paper. Headache. 2010;50(6):1089-99.
Food and Drug Administration. Drug Alerts and Statements. FDA reminds the public about the potential for life-threatening harm from accidental exposure to fentanyl transdermal systems (“patches”). April 18, 2012. www.fda.gov/drugs/drugsafety/ucm300747.htm. Accessed November 21, 2014.
Food and Drug Administration. Drug Safety and Availability. Acetaminophen Information. Last updated October 20, 2014. www.fda.gov/Drugs/DrugSafety/InformationbyDrugClass/ucm165107.htm. Accessed November 21, 2014.
Hadley G, Derry S, Moore RA, et al. Transdermal fentanyl for cancer pain. Cochrane Database Syst Rev. 2013 Oct 5;10:CD010270. doi: 10.1002/14651858.CD010270.pub2.
Hans G, Robert D, Verhulst J, et al. Lidocaine 5% patch for localized neuropathic pain: progress for the patient, a new approach for the physician. Clin Pharmacol. 2010;2:65-70.
Institute for Safe Medication Practices. Acute Care ISMP Medication Alert: FentaNYL patch fatalities linked to “bystander apathy.” we ALL have a role in prevention! August 8, 2013. www.ismp.org/newsletters/acutecare/showarticle.asp?id=55. Accessed December 1, 2014.
Institute for Safe Medication Practices. Acute Care ISMP Medication Alert: Ongoing preventable fatal events with fentanyl transdermal patches are alarming. June 28, 2007. /www.ismp.org/newsletters/acutecare/articles/20070628.asp. Accessed November 21, 2014.
Leung L. From ladder to platform: a new concept for pain management. J Prim Health Care. 2012;4(3):254-8.
Likar R, Kager I, Obmann M, et al. Treatment of localized neuropathic pain after disk herniation with 5% lidocaine medicated plaster. Int J Gen Med. 2012;5:689-92.
Llamas M. FDA sets acetaminophen dose limit, warns of liver damage. FDA News & Recalls. January 28, 2014. www.drugwatch.com/2014/01/28/fda-limits-acetaminophen-liver-damage. Accessed November 22, 2014.
Lӧtsch J, Walter C, Parnham MJ, et al. Pharmacokinetics of non-intravenous formulations of fentanyl. Clin Pharmacokinet. 2013;52(1):23-36.
McPherson ML, Uritsky TJ. Pharmacology of Pain in Older Adults: Opioid and Adjuvant. In Gloth FM, ed. Handbook of Pain Relief in Older Adults: An Evidence-Based Approach. 2nd ed. Totowa, NJ: Humana Press; 2011.
Nelson EM, Philbrick AM. Avoiding serotonin syndrome: the nature of the interaction between tramadol and selective serotonin reuptake inhibitors. Ann Pharmacother. 2012;46:1712-6.
Pasero C, McCaffery M. Pain Assessment and Pharmacologic Management. St. Louis, MO: Mosby Elsevier; 2011.
Portenoy RK, Ahmed E. Principles of opioid use in cancer pain. J Clin Oncol. 2014;32(16):1662-70.
Quinlan-Colwell A. Compact Clinical Guide to Geriatric Pain Management: An Evidence-Based Approach for Nurses. New York, NY: Springer Publishing Co; 2011.
Smith HS. Opioid metabolism. Mayo Clin Proc 2009;84(7):613-24.
Thakur R, Philip AG. Chronic pain perspectives: treating herpes zoster and postherpetic neuralgia: an evidence-based approach. J Fam Pract. 2012;61(9 Suppl):S9-15.
Trescot AM, Datta S, Lee M, et al. Opioid pharmacology. Pain Physician. 2008;11(2 Suppl):S133-53.
Vargas-Schaffer G. Is the WHO analgesic ladder still valid? Twenty-four years of experience. Can Fam Physician. 2010;56(6):514-7.
World Health Organization. WHO’s cancer pain ladder for adults. 2013. www.who.int/cancer/palliative/painladder/en/. Accessed November 22, 2014.
Ann Quinlan-Colwell is a pain management clinical nurse specialist at New Hanover Regional Medical Center in Wilmington, North Carolina.


















