Be alert to this frequently unrecognized condition.
- Hypothyroidism develops slowly over time and if left undiagnosed may put patients at risk for serious conditions, including cardiovascular disease, osteoporosis, and infertility.
- Most thyroid diseases are life-long conditions that can be managed medically.
- Primary hypothyroidism frequently is a chronic condition that requires early identification, provider monitoring, and patient adherence to medication therapy.
At her annual well visit, Linda Smith*, a 66-year-old White woman, tells her advanced practice registered nurse (APRN) that she’s gained 11 pounds without a change to her appetite or increase in caloric intake, she’s constipated, and she feels mentally foggy and increasingly fatigued over the past 6 months. Ms. Smith’s children told her that her complaints are a normal part of aging and she shouldn’t be worried. Her past medical history includes hypercholesterolemia, diabetes, and hypertension—all controlled with diet and oral medications. The APRN’s physical assessment is unremarkable. Although some of Ms. Smith’s complaints are consistent with age-related changes, the 11-pound weight gain over 6 months leads the APRN to suspect hypothyroidism.
Hypothyroidism: Stats and facts
According to the American Thyroid Association, unspecified hypothyroidism is the sixth most common diagnosis made by primary care providers in the United States. More than 12% of the U.S. population will develop a thyroid condition during their lifetime, and an estimated 20 million Americans have some form of thyroid disease. Of those, up to 60% are unaware they have the disorder. Hypothyroidism is more common in people over 60 years old, and women are five to eight times more likely than men to be diagnosed with the condition.
Hypothyroidism usually develops slowly, and when left undiagnosed, it may put patients at risk for serious conditions, including cardiovascular disease, osteoporosis, and infertility. Most thyroid diseases are lifelong conditions that can be managed medically. (See About the thyroid.)
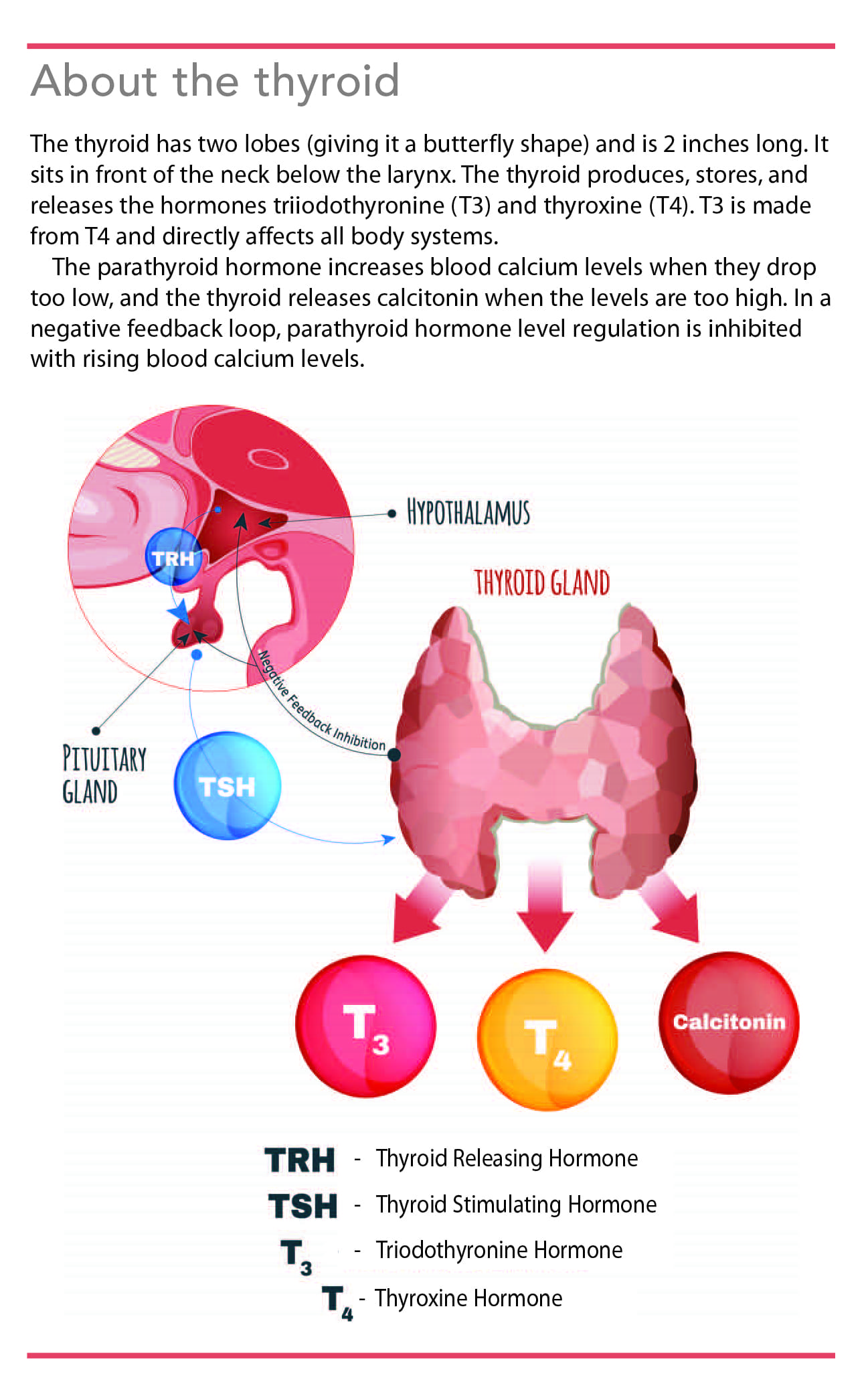
About the thyroid
The thyroid has two lobes (giving it a butterfly shape) and is 2 inches long. It sits in front of the neck below the larynx. The thyroid produces, stores, and releases the hormones triiodothyronine (T3) and thyroxine (T4). T3 is made from T4 and directly affects all body systems.
The parathyroid hormone increases blood calcium levels when they drop too low, and the thyroid releases calcitonin when the levels are too high. In a negative feedback loop, parathyroid hormone level regulation is inhibited with rising blood calcium levels.
Types and causes
In the United States, Hashimoto’s thyroiditis is the most common cause of hypothyroidism. Hashimoto’s thyroiditis is an inflammation of the thyroid gland caused by an autoimmune response to either a concurrent autoimmune disease such as rheumatoid arthritis or a familial history of autoimmune diseases. It’s characterized by an enlarged (sometimes painless) thyroid gland, throat fullness, voice hoarseness, and episodes of a sore throat or neck pain. Other causes of primary hypothyroidism include iodine deficiency; thyroid radioactive iodine therapy; surgical removal or radiation treatment of the thyroid; and certain medications, such as amiodarone, lithium, rifampin, phenobarbital, phenytoin, and carbamazepine. Subacute granulomatous thyroiditis (de Quervain’s thyroiditis), which commonly occurs in middle-aged women, is an uncommon cause of hypothyroidism.
Hypothyroidism can be differentiated into two categories, primary and secondary. Primary hypothyroidism, which accounts for 95% of hypothyroid cases, occurs when the thyroid gland itself can’t produce adequate amounts of thyroid hormone. A disease process characterized by a high serum thyroid-stimulating hormone (TSH) concentration and an insufficient amount of circulating thyroid hormones (triiodothyronine [T3] and thyroxine [T4]) causes a decrease in the patient’s metabolic rate. Thyroid function can decline slowly over time or rapidly in acute situations, such as acute illnesses, surgery, and discontinuing thyroid replacement therapy.
Secondary (or central) hypothyroidism occurs when the hypothalamus fails to produce thyroid-releasing hormone or the anterior pituitary gland fails to release thyroid-stimulating hormone, which causes the thyroid gland to release thyroid hormones. Pituitary tumors are the most common cause of secondary hypothyroidism.
Signs and symptoms
Physical examination of a patient with hypothyroidism may reveal bradycardia; hypotension; dysrhythmia; enlarged thyroid gland (goiter); puffy face; brittle nails; voice hoarseness; thinning hair; and thick, dry, flaky skin. The patient may report muscle weakness or joint pain, decreased taste and smell, depression, impaired memory, and indications of metabolism slowing such as fatigue, cold intolerance, constipation, and weight gain.
Clinical manifestations of hypothyroidism vary depending on the age of onset and the length and severity of the deficiency. In some cases, hypothyroidism symptoms mimic the normal aging process or dementia, so the patient may fail to report them or be vague in describing them to the provider. Some signs and symptoms may be so mild and nonspecific that the condition isn’t diagnosed.
Screening
Hypothyroidism screening recommendations are inconsistent, and no clear guidelines exist. The American Thyroid Association recommends that screening begin at age 35 years (and repeated every 5 years) or earlier if a family or patient history of type 1 diabetes, autoimmune disease, or neck radiation or surgery exists. The American College of Physicians suggests screening women starting at age 50 years, and the American Academy of Family Physicians recommends screening women over age 60 years. The United States Preventive Services Task Force recommends not screening asymptomatic adults of any age.
This lack of direction has led most providers to use one of two approaches: screening all individuals instead of choosing a certain age when the risk is at its highest, or screening only if the patient has clinical risk factors or if signs and symptoms are present. However, female gender and increasing age are associated with a higher prevalence of hypothyroidism.
Complications
Because hypothyroidism manifestations (such as hair thinning and cold intolerance) can mimic the aging process, it’s frequently undiagnosed in older patients. Complications of undiagnosed hypothyroidism include mental health issues that may initially manifest as irritability, but over time can lead to a flat and dull affect and depression. Other complications of hypothyroidism include infertility, birth defects, goiter, obesity, heart disease, and peripheral neuropathy. Severe hypothyroidism can result in myxedema. (See About myxedema.)
About myxedema
Myxedema (severely advanced hypothyroidism) is a life-threatening condition.
Triggers
Myxedema can be caused by
- severe hypothyroidism that’s untreated or poorly managed
- stressors (for example, acute illnesses, surgery, rapid discontinuation of thyroid replacement therapy).
Signs and symptoms
- bradycardia
- coma
- dysrhythmia
- fluid retention
- generalized edema
- hypoglycemia
- hyponatremia
- hypothermia
- hypotension
- profound lethargy
- respiratory failure
Treatment
Emergent interventions include
- maintaining airway patency
- monitoring ECG, arterial blood gases, mental status, input and output, and daily weights
- administering I.V. 0.9% sodium chloride, levothyroxine and liothyronine, glucose (as indicated), and corticosteroids.
Diagnosis
Obtaining a complete history (symptoms and duration) and performing a comprehensive physical examination are necessary to rule out other diagnoses. For example, fatigue may suggest a sleep issue, anemia, depression, chronic fatigue syndrome, or possible age-related changes. Constipation, weight gain, and mental fogginess may be related to a lack of activity secondary to fatigue.
For patients suspected of having hypothyroidism, a serum TSH is the initial test. If the result is elevated, the TSH is repeated along with a T4 to make a definitive hypothyroidism diagnosis. A thyroid antibody test is added if Hashimoto’s disease is suspected as the cause, or if there is current or history (patient or familial) of autoimmune disease or swollen thyroid gland (See Diagnostic tests.)
Diagnostic tests
For patients suspected of having hypothyroidism, serum thyroid function (including thyroid-stimulating hormone [TSH], triiodothyronine [T3], and thyroxine [T4]) and thyroid antibody tests are performed.
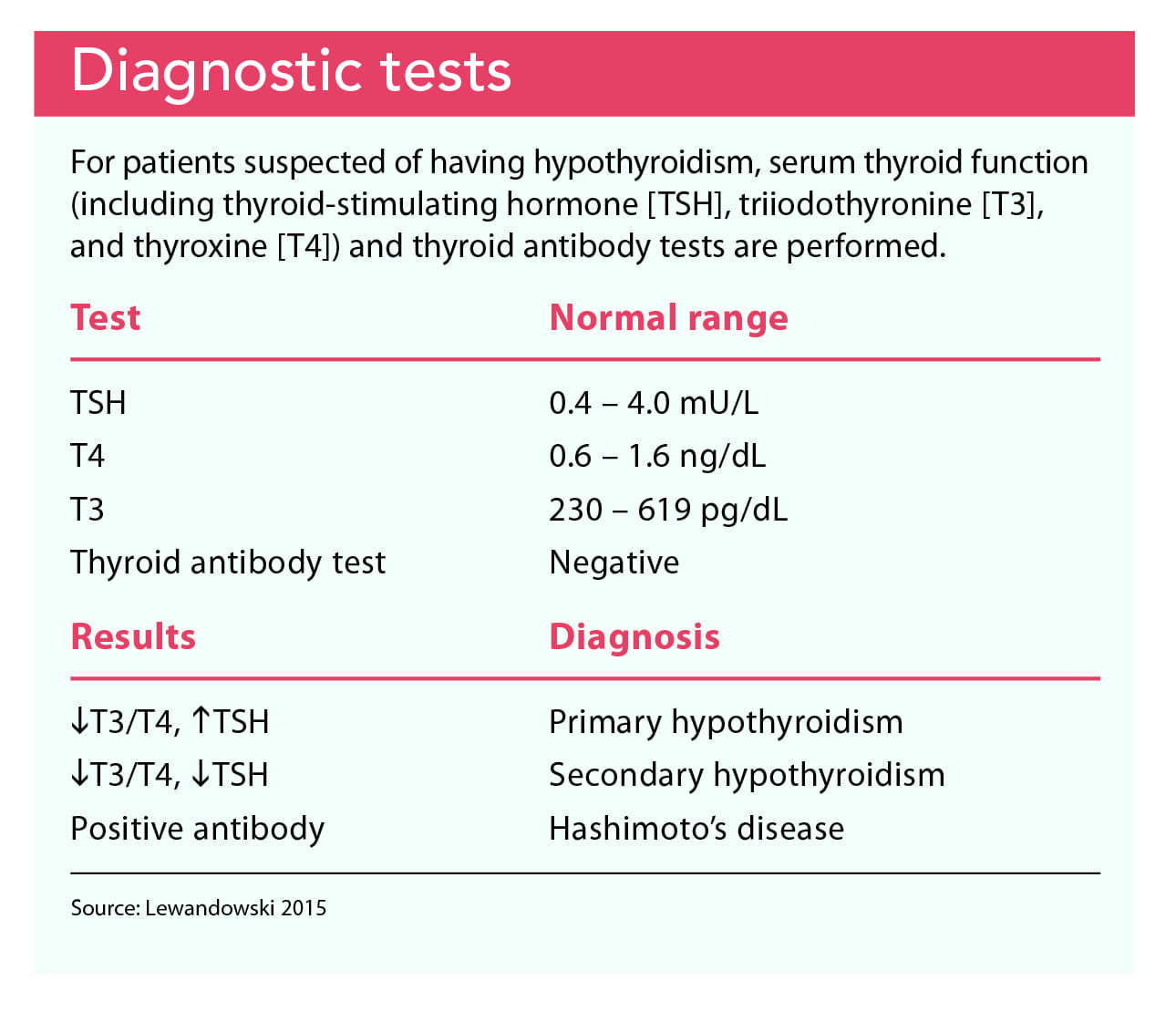
Because of Ms. Smith’s symptoms, her APRN adds TSH levels to her blood work order. All results are within normal range except for TSH, which is 7.6 mU/L (normal is 0.4 to 4.0 mU/L). A repeat TSH and a T4 are completed at a follow-up visit; the results are TSH 7.7 and T4 0.3 ng/dL (normal is 0.6 to 1.6 ng/dL). A thyroid antibody test isn’t performed because the physical exam shows Ms. Smith’s thyroid is normal in size.
Treatment
Primary hypothyroidism is treated with levothyroxine, a synthetic thyroid hormone replacement. The exact dose depends on the patient’s age, weight, and severity of the disease; the presence of any comorbidities; and current medications that may interfere with how well the body absorbs levothyroxine. According to the manufacturer, the levothyroxine dose should be adjusted based on serum TSH levels, which are measured after initial treatment. The dose is adjusted every 6 to 8 weeks until TSH and T4 levels are reduced to normal ranges and the patient’s thyroid is functioning properly.
After reaching a therapeutic levothyroxine dose, TSH and T4 are measured every 6 months to 1 year. Although TSH and T4 may be in normal ranges, mild symptoms may be present, requiring slight dosage increases. Levothyroxine should be taken on an empty stomach to avoid diminishing its absorption. Ideally, the medication should be taken between 5:00 am and 6:00 am to provide consistency and mimic the diurnal pattern of T3 and T4 release from the thyroid gland.
The APRN orders levothyroxine 12.5 mcg/day because of Ms. Smith’s age and medical history. When a TSH is repeated in 7 weeks, it’s within normal range; Ms. Smith reports that her symptoms are subsiding and she’s lost 4 pounds.
Nursing considerations
To evaluate the effectiveness of hypothyroidism pharmacotherapy, ask patients about their symptoms. Indications of improvement include increased activity tolerance, better mental clarity, and daytime wakefulness. Monitor patients’ TSH and T4 levels as well as their blood glucose levels (especially in patients with a history of diabetes because levothyroxine can increase the metabolic rate resulting in altered glucose use) as ordered. Instruct patients to check their weight once a week; it should remain stable, but they may lose some weight as the treatment increases their metabolism. In addition, monitor patients for treatment adherence.
Primary hypothyroidism treatment is lifelong and requires pharmacotherapy and thyroid function assessment. To avoid medication issues, and for consistent absorption, provide patient education.
- Take levothyroxine on an empty stomach, ideally between 5:00 am and 6:00 am, with a full glass of plain water.
- Levothyroxine has a long half-life and may take up to 6 weeks to be fully effective.
- Avoid proton pump inhibitors and calcium and magnesium supplements. However, if any of these medications are required, they should be taken 4 hours before or after levothyroxine.
- Don’t abruptly discontinue levothyroxine. Any dosage change must be discussed with your provider.
- If you miss a dose, take it as soon as possible. If it’s almost time for the next dose, skip the missed dose and return to a regular dosing schedule. Don’t double dose.
- Your blood thyroid function (TSH and T4) will be monitored, and your levothyroxine dosage may be adjusted until symptoms subside or are significantly reduced.
- Immediately report these danger signs to your provider: irritability, chest pain, heat intolerance, insomnia, rapid weight loss, dysrhythmia (irregular heartbeat), and tachycardia (racing heart).
Be alert
Primary hypothyroidism is a chronic condition that requires early identification, provider monitoring, and patient adherence to pharmacotherapy. Screening recommendations are inconsistent, so nurses must be alert to hypothyroid signs and symptoms and advocate for appropriate testing to confirm a diagnosis and ensure proper treatment to prevent further metabolic complications.
At a follow-up visit, the APRN provides Ms. Smith with additional patient education, including that she check her weight once a week. The APRN explains that Ms. Smith will experience some weight loss as treatment increases her metabolism but that she should call the office if she notes a significant weight gain without diet changes. In addition, the APRN explains that regular blood work may be required until a therapeutic medication level is reached and then measured every 6 months to 1 year. AN
*Name is fictitious.
To view a list of references, visit myamericannurse.com/?p=70040.
MaryAnn D’Alesandro is an assistant professor of nursing at the University of Tampa in Tampa, Florida.
References
American Thyroid Association. General information/press room. thyroid.org/media-main/press-room/
ATI Nursing Education. RN Adult Medical Surgical Nursing Review Module. 11th ed. Leawood, KS: ATI; 2019.
Definitive Healthcare. 10 most common diagnoses and procedures in primary care. August 13, 2020. bit.ly/34lD4DF
Fitzgerald PA. Endocrine disorders. In: Papadakis MA, McPhee SJ, Rabow MW, eds. Current Medical Diagnosis and Treatment 2018. 57th ed. New York City, NY: McGraw-Hill Education; 2018; 1117-21.
Hinkle JL, Cheever KH. Brunner & Suddarth’s Textbook of Medical-Surgical Nursing. 13th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2013.
Khowaja N. Evidence based nursing guidelines of adult patients with hypothyroidism. International Conference on Thyroid Disorders and Treatment; February 2016; Philadelphia, PA. longdom.org/proceedings/evidence-based-nursing-care-guidelines-of-adult-patients-with-hypothyroidism-6025.html
LeFevre ML, U.S. Preventative Services Task Force. Screening for thyroid dysfunction: U.S. Preventive Task Force recommendation statement. Ann Intern Med. 2015;162(9):641-50.
Lewandowski K. Reference ranges for TSH and thyroid hormones. Thyroid Res. 2015;8(suppl 1):A17.
Mayo Clinic. Hypothyroidism (underactive thyroid). mayoclinic.org//diseases-conditions/hypothyroidism/symptoms-causes/syc-20350284?p=1.
National Institute of Diabetes and Digestive and Kidney Disorders. Hypothyroidism (underactive thyroid). August 2016. niddk.nih.gov/health-information/endocrine-diseases/hypothyroidism#common
Patil N, Rehman A, Jialal I. Hypothyroidism. StatPearls. August 10, 2020. ncbi.nlm.nih.gov/books/NBK519536
Simon C, Weidman-Evans E, Allen S. Subclinical hypothyroidism: To treat or not to treat? J Am Acad Physician Assist. 2020;33(5):21-6.
Trimboli P, Scappaticcio L, De Bellis A, et al. Different formulations of levothyroxine for treating hypothyroidism: A real-life study. Int J Endocrinol. 2020(4524759):1-5.
West V, Felz MW. Hypothyroidism: A clinical case review. Clinical Advisor. January 10, 2020. clinicaladvisor.com/home/topics/endocrinology-information-center/hypothyroidism-a-clinical-case-review