How to build a case that creates improved patient outcomes.
In this new, unpredictable healthcare universe, chief nursing officers (CNOs) and chief financial officers (CFOs) are jettisoning preconceived notions of their individual roles and finding innovative ways to work together to create better outcomes.


Experts in acuity-based staffing discussed how CNOs and CFOs can come together over this shared goal during the webinar “CFO/CNO partnership for workforce management outcomes: Benefits of acuity-based staffing,” hosted on July 12, 2017, by American Nurse Today, API Healthcare, and Intel. Lillee Gelinas, MSN, RN, CPPS, FAAN, editor-in-chief for American Nurse Today, moderated the program, which built on the 2016 webinar “Practical steps for applying acuity-based staffing: What nurse leaders need to know.”
“Finance and nursing executives face many uncertainties in today’s healthcare environment, but one factor still under their control is the cost of labor,” said Gelinas. “An investment in labor is an investment in quality, but like any other transaction, hospital leaders want the best return from their dollars.”
Acuity-based staffing is a valuable tool for maximizing those returns because it ensures the right staff are in the right place at the right time—essential goals as healthcare leaders face a worsening nursing shortage and continuing demands to do more with less.
“Acuity-based staffing is an initiative that affects all areas of importance to the CFO, the CNO, and the entire organization,” said Karlene M. Kerfoot, PhD, RN, NEA-BC, FAAN, chief nursing officer, API Healthcare, Workforce Management. “It impacts financial outcomes, clinical outcomes, patient satisfaction, and staff satisfaction.”
Kerfoot’s copresenters, Jack Needleman, PhD, FAAN, Fred W. and Pamela K. Wasserman Professor and Chair in the department of health policy and management at the UCLA Fielding School of Public Health and Sylvain (Syl) Trepanier, DNP, RN, CENP, chief nursing executive for Providence St. Joseph Health, California (LA Market), agreed that acuity-based staffing is the best tool available to calculate the most accurate combination of RNs needed to produce good clinical outcomes while also containing labor costs.
Before CNOs can build the business case for acuity-based staffing, however, they need to understand CFOs’ concerns and needs.
What CFOs want


According to a 2017 survey of 75 CFOs by Becker’s Healthcare, CFOs’ top concerns are managing labor costs (73%), monitoring the uncertainty surrounding reimbursements (71%), and staying competitive in the healthcare market (61%). “We know that anywhere from 40% to 60% of a healthcare organization’s budget is labor cost,” Kerfoot said.
Hurdles to workforce management identified in the survey include:
- flexing staff up and down based on the number of patients and their needs at any one time (60%)
- managing overtime and premium labor costs to prevent bringing in outside staff (47%)
- leveraging staff across the organization (45%)
- staffing productivity as a lagging measure rather than using proactive scheduling (43%)
- managing staff turnover and the cost of orienting new personnel (40%).
The survey also shows that CFOs believe clinicians aren’t using all the data that’s available to them through the investment of millions of dollars in electronic health records (EHR). For example, data on admissions, discharges, and transfers; staff skill and competency; and patient acuity, to name a few, aren’t being fully used, Kerfoot said. (See Underutilization of data.)
Underutilization of data |
| A survey of 75 chief financial officers conducted by Becker’s Healthcare identified that many health systems aren’t taking full advantage of data in making staffing decisions. |
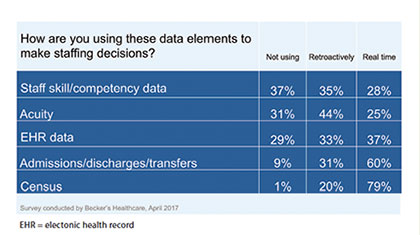 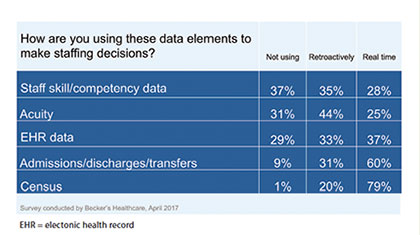 |
Failure to use that data may result in patient harm because the right number of staff with the right qualifications might not be available to deliver the care patients need.
The evidence: Missed care leads to bad outcomes
Many studies have shown that sufficient nursing staff leads to improved clinical outcomes without unreasonably increasing a healthcare organization’s budget, Needleman said. Research also has shown that bad outcomes are caused in large part by “missed care” or “care left undone.”
“What we see in hospitals staffed at low levels that no one should be comfortable about is that reported levels of missed care are quite high,” Needleman said. “So, missed care represents one of the clear pathways by which inadequate staffing leads to poor patient outcomes.”
Indeed, a measure of RN understaffing is nurses’ inability to get their work done during a normal shift. Studies show time and again that adequate staffing on nursing units allows RNs to complete all their work, not just most of it. This includes the visible physical tasks, such as taking vital signs and administering medication, and the unseen and less measurable cognitive nursing responsibilities, such as:
- interpreting changes in a patient’s condition and deciding on the appropriate response
- identifying incorrect physician orders
- catching medication errors
- coordinating patient care
- educating and preparing patients and their families for self-care
- providing emotional support.
Together, these actions reduce infections and complications, prevent medical and nursing errors, help reduce readmissions, and lead to patient and staff satisfaction, Needleman said.
Needleman noted there are at least three dimensions to accurate staffing:
- patient characteristics and the critical issues influencing the proper staffing level
- nurse characteristics
- unit and organizational factors, such as turnover and efficiency of support services.
If a CFO or chief executive officer asks if the institution can afford adequate staffing, the answer is that management needs to consider not only the direct costs of nursing but also the cost offsets of adequate staffing that come from shorter length of stay, reduced adverse events, reduced readmissions, and missed care, Needleman said. (See Cost benefits of adequate staffing.)
Cost benefits of adequate staffing |
| Increasing the proportion of RNs and their number of hours reduces adverse outcomes and even patient deaths as the data analysis below shows. |
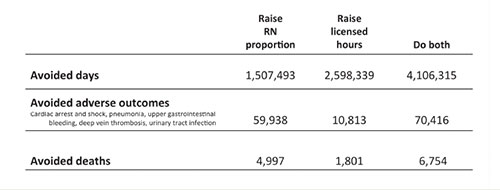 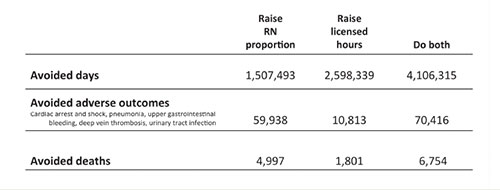 |
| Although these staff changes incur costs, those costs are clearly offset by the savings achieved in improved outcomes, as noted below. |
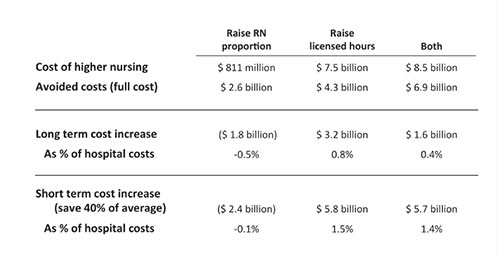 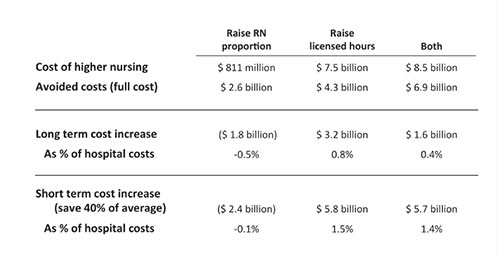 |
| Source: Needleman J, Buerhaus PI, Stewart M, Zelevinsky K, Mattke S. Nurse staffing in hospitals: Is there a business case for quality? Health Aff. 2006;25(1):204-11. |
One of the key messages of a business case analysis is that increasing RN staffing hours may cost a little more but will pay for itself by avoiding adverse outcomes. Trying to save money by de-skilling the nursing staff, by reducing or replacing RNs with LPNs or other less-skilled staff, is likely to increase the budget’s net cost, not save money, Needleman said.
In summarizing a business case for an interoperable acuity-based system, he recommended pointing out to CFOs that:
• Nursing is a core service line of hospitals, not just a cost center, and should be assessed as a service line.
• Patients expect, and have a right to expect, that their nursing care will be safe, reliable, and effective.
• Nursing care depends on staffing at adequate levels to meet patients’ needs.
• Acuity-based systems, whether commercial or locally developed, can ensure more appropriate levels of staffing matched to patient acuity and needs.
Hospital executives must understand that nurses completing “most of their work” is not acceptable and certainly not worth the savings, Needleman emphasized.
Developing effective CNO and CFO relationships
Before presenting evidence such as Needleman outlined, the CNO has to build an effective partnership with the CFO. As challenging as it may seem, a CNO may need to take the first step toward breaking down traditional organizational silos and establishing a relationship with a CFO, Trepanier said. Here are some ideas to get you started:
- Be thoughtful and intentional when reaching out to your CFO. Don’t make just a passing effort. Show interest in the CFO rather than trying to be the subject of interest. As in all effective relationships, be honest and avoid gossip or innuendo.
- Don’t ask for something at the start of the relationship. Instead, as the relationship builds, look for common areas of concern and then suggest an issue you could work on together.
- Be prepared to respond thoughtfully and not react emotionally. Conversations with CFOs may not always go as smoothly as you’d like. Think about how you emotionally feel about an issue before you start a particular conversation with a CFO. Review your rationale. In other words, Trepanier said, don’t “shoot before you aim.”
- Ask if there’s an institutional business case model that you can familiarize yourself with.
As you feel more confident in the relationship, approach the CFO about the need to implement an interoperability acuity-based staffing system. Present the idea in chunks at different times, not all at once. Ask if you can work on it together and suggest that you start developing the business case for the system, Trepanier said.
If you’ve never built a business case, it’s time to learn. “Creating a business case is a skill that you need to develop as a CNO,” Trepanier said. Your institution may have a model it recommends. If not, search for outside resources and tools, such as Build Your Business Plan, to help you learn.
Trepanier recommended including the following in the business case: the connection to the organization’s vision and mission, a clear description of the problem, a detailed explanation of the solution, expected outcomes and how they’ll be measured, and the value contribution, which also should tie in to the vision and mission.
After a business case is developed in collaboration with the CFO, Trepanier suggested identifying like-minded coworkers and talking to them about your plans. Winning support from influential stakeholders who can support you during the official presentation to top leadership is an advantage. They also may give you ideas to strengthen your business case.
Your business case should include these tangible benefits of an acuity-based system:
- fulfills any regulatory requirements in your state
- provides an accurate, objective picture of patients’ needs and the workload associated with them
- supports individualized staffing plans based on patients’ needs
- promotes a budget based on actual patients’ needs as opposed to the “historical” hours per patient, per day now used in many hospitals.
Selecting an acuity-based staffing system
Your business case will include one of two types of acuity-based staffing systems—commercial or local. Needleman said that both have pros and cons. When choosing a system, keep in mind that it should be able to formulate correct staffing mix with minimal additional work by hospital staff. To do so, the system should have indicators that measure patient complexity, optimal required nursing care, available resources, and relevant organizational attributes. And it should truly reflect nursing work.
Commercial systems come with an existing algorithm and can be calibrated to the organization’s nursing model. In general, commercial systems tend to have a high data-entry burden, although this can be mitigated by linkages to EHRs. Local systems take into account the nature of the patients who are typically on specific units, but the data-entry burden also can be high and most local systems don’t have links for tracking data entry and storage.
Data plus automation equals better staffing
The selected acuity-based system needs to be integrated into workforce management to facilitate effective decision-making. “We have data absolutely everywhere, but the problem is that no human being can absorb all the data and synthesize it into a coherent formula upon which to make decisions,” Kerfoot said. Automated acuity-based staffing systems support the transformation of data into information that nurse managers and CNOs can use to determine appropriate staffing levels. The system should incorporate patient data, staff data, and operations data to develop a staff scheduling plan that CNOs and CFOs agree meets their needs and their patients’ needs. Automated tools and processes help ensure that the right data (patient, staff, and operations) get to the right people at the right time to drive better workforce management systems and clinical outcomes.
“Intelligent staffing,” as Kerfoot refers to it, depends on staffing optimization, which is the ability to fully leverage the nursing staff’s time and talent to meet patients’ needs. It’s also the ability to flex staff up and down before and during a shift as unexpected changes happen.
Having a more accurate assessment of your staffing needs will help eliminate chaos down the road by not having to call in a staff member from home to help with a unit’s unexpected uptick in census, Kerfoot said. Experience has taught nurses that the kind of care patients need can’t be determined with a census number alone. Each patient is different. Some need complete care, while others are almost self-sufficient. Some patients have numerous lines and medications, while others are ready to go home. Information about individual variations for nursing care determines the actual nursing time needed.
And just as each patient is different, so too are the caregivers. Each nurse has his or her own set of skills, education, experiences, preferences, and availability.
Staffing needs also are affected by unit dynamics, such as admissions, discharges, and transfers. And life is unpredictable. Patients crash, develop unpredicted allergies to medications, or fall and break a bone. Staff members call in sick or need to leave because a child is ill.
When data about patient needs, individual RN characteristics, and unit dynamics are considered together, a complete picture of staffing needs is revealed.
Building optimization
Optimizing staff consists of creating the schedule, fostering open shift management, making intrashift adjustments, and conducting a postshift analysis. (See Optimizing staff.)
Optimizing staff |
| Optimizing nursing staff requires looking ahead at anticipated needs, being nimble during a shift, and reviewing past performance. |
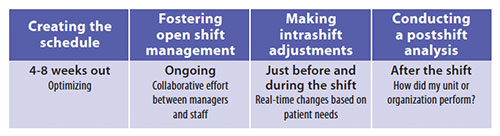 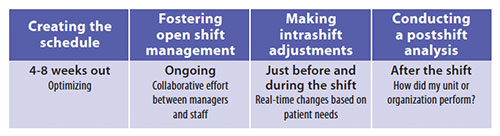 |
Creating the schedule should start 4 to 8 weeks out. Base the schedule on a staffing matrix that is, in turn, based on the budget. The more accurate the staffing matrix is, the sooner an accurate schedule can be created. Be sure to look at available predictive information. This may include seasonal acuity, such as the start or end of the flu season, summer in the city when violence increases, or an upcoming holiday.
Equity rules also are important, ensuring that employees are all treated fairly and consistently when it comes to factors such as working holidays and having access to self-scheduling. Fairness in patient assignments is important for patient outcomes and staff engagement.
A comprehensive schedule creation process is essential because the more complete and accurate the schedule is, the fewer adjustments will be needed as the schedule period gets closer.
Fostering open shift management promotes collaboration between nurse managers and staff across the enterprise so that patient care needs are met within budget constraints, while minimizing the amount of effort required to fill shifts. “We want to make sure that we have visibility across the system so that one person can look at what is available on another unit to see if sharing a staff member can relieve a shortage somewhere else,” Kerfoot said.
By breaking down staffing silos between units and departments and expanding visibility to use workforce resources more effectively, shifts are filled quickly and cost effectively, with the best available resources. Staff become more engaged in the process because they have more input into their schedule, which in turn boosts morale.
Making intrashift adjustments should occur just before and during the shift and be based on evolving patient needs. As one health system CNO explained to Kerfoot, “We use data, data, data. Information from our EHR is fed into our acuity system every 2 hours and staffing is adjusted every 4 hours based on this data. Managers monitor nurse-patient assignments and staffing multiple times a day and make adjustments.”
Conducting a postshift analysis is something CNOs are familiar with, but optimization requires a more dynamic approach. In the past, most hospitals used data compiled after the shift (or even worse, data that’s available only after the end of the pay period) to take a retrospective look at their organization’s productivity, use of overtime, and other labor metrics. This is sometime referred to as a rearview mirror approach—you can see where you’ve been, but it’s not helpful for making decisions about where you need to go.
With a dynamic staffing model, managers can focus on using relevant data before, during, and after each shift to make proactive adjustments that have a meaningful impact on financial and clinical outcomes. Retrospectively, it allows CNOs and CFOs to review whether the staffing and acuity matched what was expected compared to the allotted budget. If it didn’t, they can determine what changed and why.
For example, by looking at the shifts a nurse has already worked, as well as the shifts he or she is scheduled to work, overtime can be projected and changed before it is incurred. When the focus is on making the right adjustments before and during each shift, the after takes care of itself, with no unpleasant surprises.
An effective process
How can leaders ensure staffing meets patients’ needs while balancing the budget? The answer is clear: Understanding the value of acuity-based staffing, forging partnerships between CFOs and CNOs to implement this form of staffing, and integrating it into the organization’s workforce management process will promote patient safety and ensure fiscal responsibility.
Janet Boivin is a freelance writer.
Editor’s note: Access a recording of the webinar.


















