N ursing has a powerful positive impact on patients’ lives. Because of its intimate nature, as exemplified by the essence of nursing, nurses can make the most significant contribution to patients’ experiences, safety, and healing.
The spirit and spirituality we express through our nursing care reflects the very core of organizational culture. A culture of caring is marked by a sound professional practice functioning within an innovative environment to improve patient and community health. Today, with such a strong evidence base in place to demonstrate the correlation between nursing and outcomes, a caring culture also can be described as a culture of curing—but not curing in the most obvious clinical sense. High-quality nursing care thriving in a healthy work environment can cure healthcare-related economic woes through better outcomes achieved at lower cost. With this type of caring—and curing—culture, nurses, and nursing practice thrive.
“We’ve never done it that way before”
How do we ensure that a caring, curing culture that nurtures both nurses and nursing practice survives the current winds of change while preserving the essence of nursing? It starts with understanding the type of culture that’s driving the work environment and the staff working in it.
Frequently, culture is described as “what happens when no one is watching,” where the strongest forces that drive nursing practice reflect the attitude that “We’ve always done it that way.” In reality, nursing evolves continuously. Some changes occur gradually and may not be readily apparent. These changes are similar to updates for smartphone apps: We accept the update, install it, and don’t need a lot of training to use the new version. In other words, the same work environment and culture that was in place before the change stays in place.
But other changes are more obvious and abrupt, causing the evolution to feel more like a revolution. The resulting transformation can be dramatic, redesigning the work environment as a place nurses and patients might not recognize. Examples include eliminating the centralized nursing station and implementing new technology that changes the world at warp speed, such as robotics. Such dramatic changes can be good, and many come about through innovation. These changes take us from “We’ve always done it that way” to “We’ve never done it that way.” They can be exciting, igniting the spirit of caring and fanning the flame even more.
George Bernard Shaw said, “You see things; and you say ‘Why?’ But I dream things that never were; and I say ‘Why not?’” When it comes to today’s consumers and the economic demands on healthcare organizations, we obviously need to design new ways of caring, including new ways of caring for both patients and caregivers. This change must take place within the context of high-performance work environments with inspirational cultures. The need for speed and an open mind to create and achieve new ways is crucial. So the next time someone says, “We’ve never done it that way,” you might want to ask, “Why not?”
Ethics, work environment, and impact on caring
Change is all around us, and our response to it determines the level of success we can achieve. Understanding the impact of change and innovation on care and the caregiver is important. Lack of understanding or inability to address the challenges can undermine even the healthiest work culture.
The links between ethics and caring are well-known. However, we’re often hesitant to address moral and ethical issues as soon as the need arises. The result is a drain on both staff and the caring culture. The American Nurses Association’s (ANA’s) Ethics Advisory Board believes an ethical environment or climate is necessary for a healthy work environment: You can’t have one without the other. ANA’s Code of Ethics for Nurses with Interpretive Statements (2015) reflects the nursing profession’s ethical values and obligations. A nonnegotiable ethical standard, it serves as an expression of nursing’s commitment to society.
Two provisions in the Code of Ethics offer important guidance related to the need for an ethical environment and a safe, healthy culture:
- Provision 5: The nurse owes the same duties to self as to others, including the responsibility to promote health and safety, preserve wholeness of character and integrity, maintain competence, and continue personal and professional growth.
- Provision 6: The nurse, through individual and collective effort, establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care.
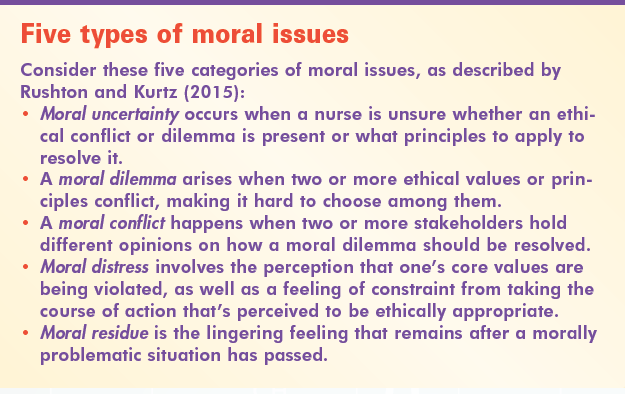
This guidance is particularly important when dealing with ethical and moral issues that may arise at any time while delivering nursing care. (See Five types of moral issues.)
ANA defines a healthy work environment as one that is safe, empowering, and satisfying. It’s not just the absence of real and perceived threats to health but a place of physical, mental, and social well-being, supporting optimal health and safety. In healthy workplaces, moral and ethical issues are understood and addressed, and the health and safety of patients and healthcare workers are respected and continuously promoted. In these workplaces, the essence of nursing emerges, reflecting the art of caring, the science of curing, and the soul of our profession.
Selected references
American Nurses Association. Code of Ethics for Nurses with Interpretive Statements. Silver Spring, MD: Author; 2015. nursingworld.org/MainMenuCategories/EthicsStandards/CodeofEthicsforNurses/Code-of-Ethics-For-Nurses.html
Rushton CH, Kurtz MJ. Moral Distress and You: Supporting Ethical Practice and Moral Resilience in Nursing. Silver Spring, MD: American Nurses Association; 2015.
Lillee Gelinas is Editor-in-Chief of American Nurse Today and system vice president and chief nursing officer of Clinical Excellence Services at CHRISTUS Health in Irving, Texas. She wishes to thank Beckett Gremmels, PhD, System Director of Ethics, CHRISTUS Health, for his research assistance for this article.



















7 Comments.
Caring does help cure. Being kind, patient and having the ability to take time to listen to our patient and their needs goes along way. Connect with our patients and staff to improve outcomes.
Interesting. Maybe someone already have policies for that.
I think its important that this article addresses the nurse’s ethical obligation in providing for a safe environment for our patients. Provision 5 of the ANA’s code of ethics is interesting as it says we as nurses owe ourselves the same concern for care as we provide to our patients. It is so easy to forget to take care of oneself when we are constantly concerned with and putting priority on others’ safety and care day in and day out.
I work in the Behavioral Health setting where it seems we have always said “no” to patients in an attempt to keep them safe and it seems sometimes control them. My hospital has started a new campaign of “just say yes” in which nurses look at each patient request independently in deciding on responses to patient requests.
yes, I agree. The spirit and spirituality and indeed the positive energy that we express and exude in the process of administering care to our clients/ patients go a long way to aid in their healing. Healing process starts from the mind, and if the environment is charged with the right energy which the nurse is integral part of then one can say that the curing of the patient starts from then.
Great! This is wonderful. We’re very thankful!
Eye-opening!!! Best wishes!
Does this article havi a doi?
Thank you,
Staci