This nursing role supports sepsis protocol improvements.
- Each year, over 1.7 million adults in the United States develop sepsis and 350,000 die from it.
- Sepsis bundle adherence is associated with lower 30-day mortality rates.
- Many acute care hospitals lack processes and resources to effectively and efficiently navigate sepsis patients.
Without timely intervention, sepsis (a life-threatening medical emergency that occurs when an infection triggers a chain reaction) can result in tissue damage, organ failure, and ultimately death. Although the most common causes of sepsis are bacterial infections, viral infections—such as COVID-19, influenza, and fungal infections—also can result in sepsis.
Each year, over 1.7 million adults in the United States develop sepsis and 350,000 die from it. In the acute care setting, one-third of overall hospital patient mortalities involve a sepsis diagnosis, although most develop before hospitalization. (See Risk factors, signs, and symptoms.)
Sepsis identification: A race against time
Helping patients survive sepsis
Risk factors, signs, and symptoms
The following factors place individuals at higher risk for sepsis:
- Age: Adults ≥65 years and children <1 year
- Chronic conditions: Cancer, diabetes, lung or kidney disease
- Exposure: Past survivors of sepsis and those with recent hospitalizations
- Immune system: Individuals with weakened immune systems and those who’ve had a recent illness
Signs and symptoms of sepsis include the following:
- Confusion or disorientation
- Elevated heart rate or weak pulse
- Extreme pain or discomfort
- Fever, chills, clammy skin
- Shortness of breath
The problem
For years, sepsis has remained the purview of intensivists and infectious diseases specialists. In the acute care setting, deteriorating patients might go unrecognized and interventions administered too late. Several recent developments aim to address these issues.
The Centers for Medicare and Medicaid Services (CMS) worked with purchasers, physicians, healthcare organizations, and consumers to identify evidence-based process measures (core measures) to reduce morbidity, mortality, variability, and cost while improving quality outcomes. In 2015, CMS and The Joint Commission (TJC) launched a sepsis core measure for all TJC-accredited U.S. hospitals (jointcommission.org/measurement/measures). CMS outlined appropriate treatment for these patients and initiated compliance tracking. CMS reviews organizations’ compliance with the sepsis early management bundle (SEP-1) for inpatients, age 18 and over, with an ICD-10-CM Principal or Other Diagnosis Code of sepsis, severe sepsis, or septic shock.
Patients who qualify for the SEP-1 early management bundle must receive all of the components within the bundle, or the treatment is considered noncompliant. (See SEP-1 bundle components.)
SEP-1 bundle components
The sepsis early management bundle (SEP-1) requires implementation of the following interventions within 3 hours of the onset of sepsis symptoms:
- Measure initial lactate level.
- Draw blood cultures prior to antibiotics.
- Administer broad-spectrum or other antibiotics.
AND within 3 hours of initial hypotension OR within 3 hours of severe sepsis or septic shock if systolic blood pressure <90 mmHg or mean arterial pressure <65 mmHg, implement the following:
- Resuscitate with 30 mL/kg crystalloid fluids.
AND within 6 hours of presentation of severe sepsis or septic shock ONLY if the initial lactate is elevated, perform the following:
- Repeat lactate level measurement.
AND within 6 hours of severe sepsis or septic shock presentation, ONLY if hypotension persists after fluid administration, implement the following:
- Administer vasopressors.
- Repeat volume status and tissue perfusion assessments.
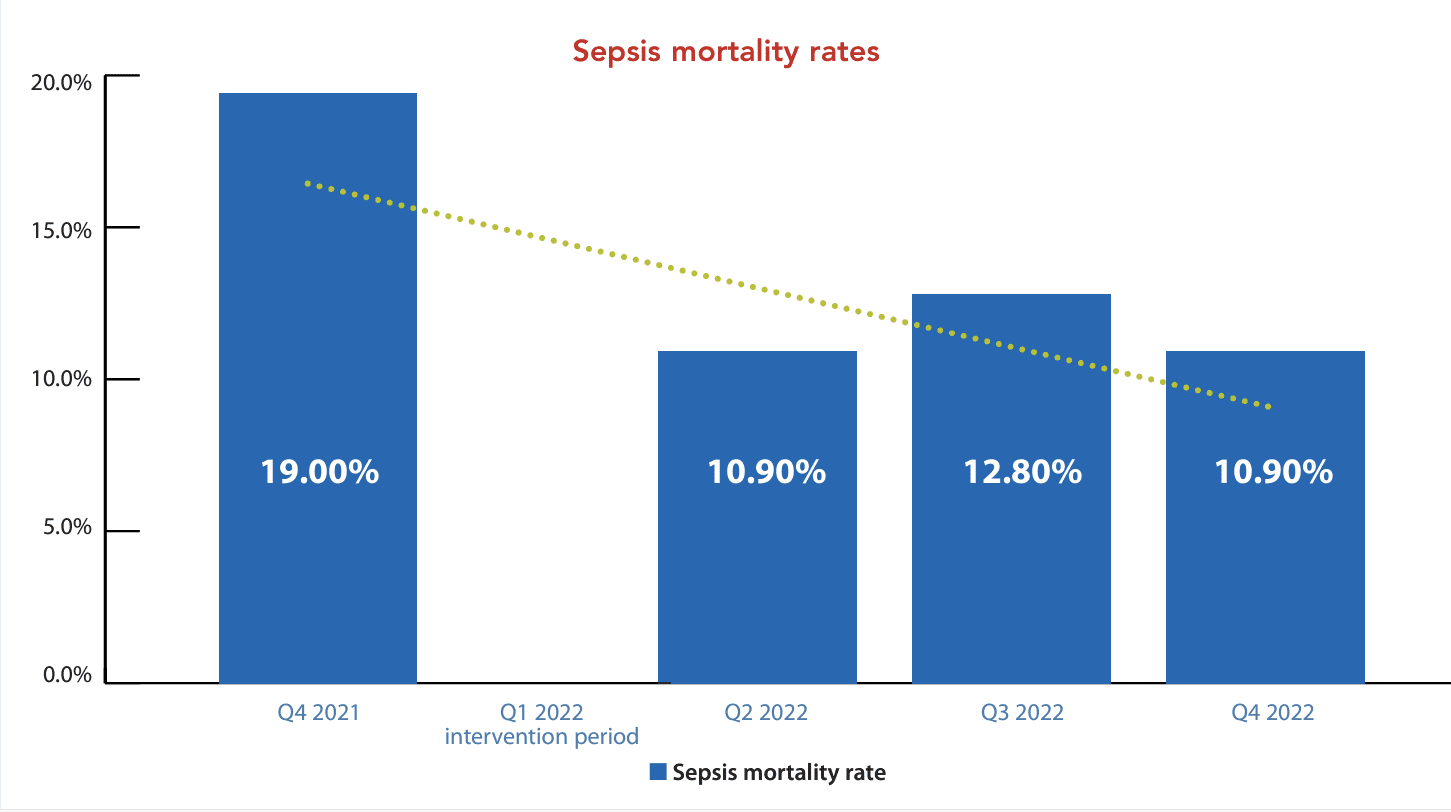
Townsend and colleagues found an association between SEP-1 bundle compliance and lower 30-day mortality rates; thus, improving compliance may reduce the incidence of avoidable deaths. However, many acute care hospitals lack processes and resources to effectively and efficiently navigate sepsis patients.
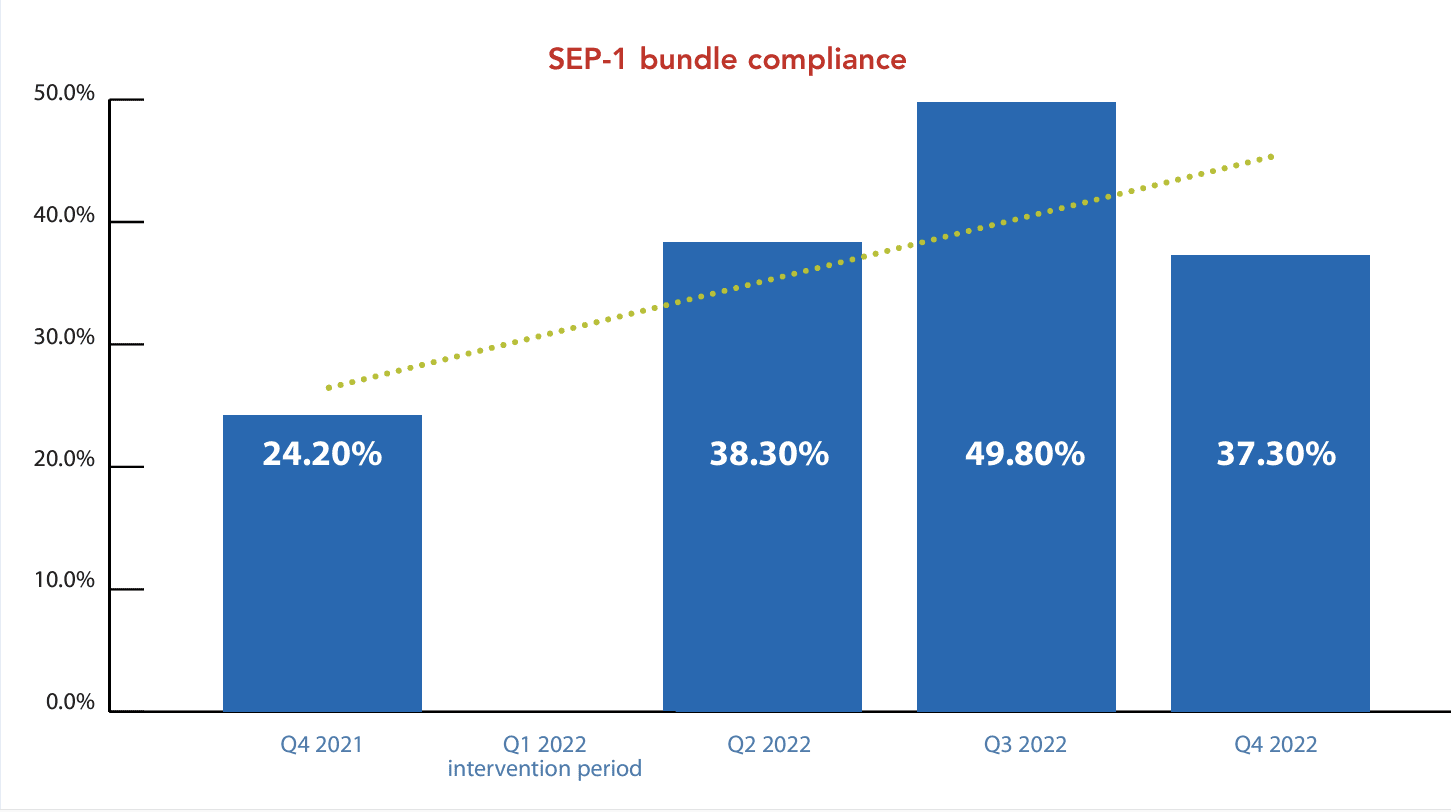
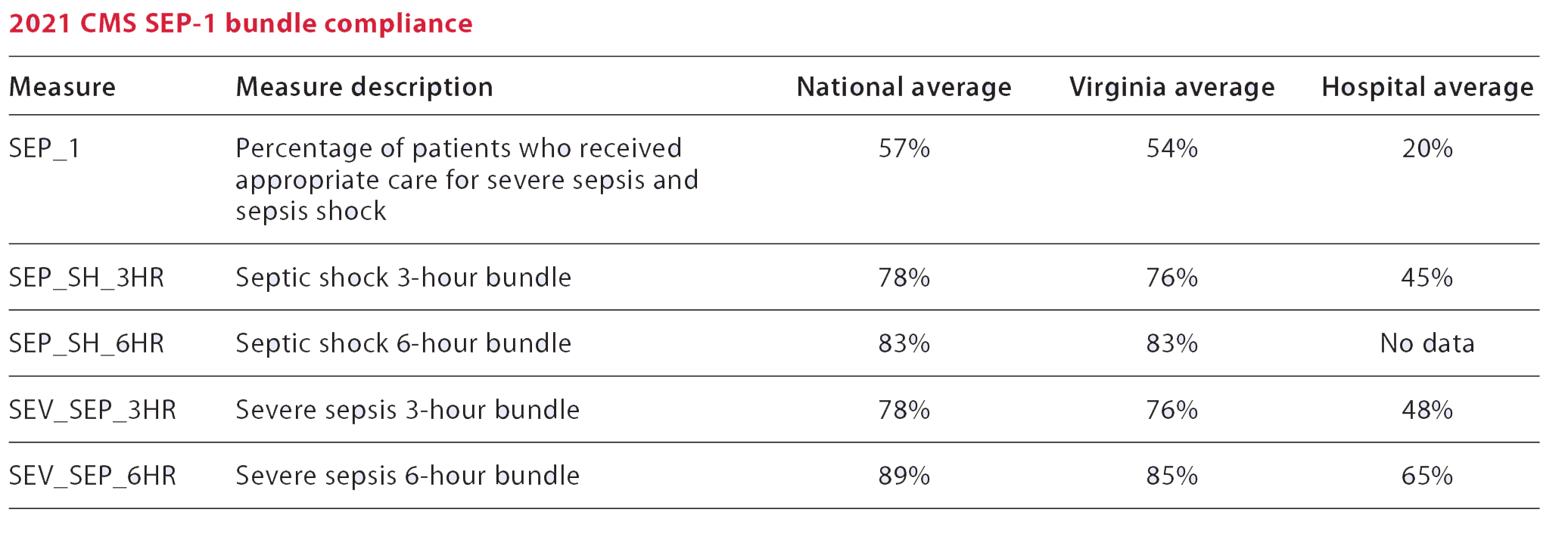
In 2021, compliance with these core measures at our 250-bed acute care hospital in southeastern Virginia ranked significantly below state and national averages. To improve hospital sepsis mortality rates and sepsis bundle compliance, a team of nurse leaders at this multi-designated Magnet® hospital reviewed best practices to improve processes and reduce sepsis mortality rates. (See Bundle compliance.)
Bundle compliance
In 2021, our acute-care hospital’s compliance with the Centers for Medicare and Medicaid Services (CMS) sepsis early management bundle (SEP-1) was well below national and state averages.
What we learned
A literature review revealed an evidence-based approach for improving early sepsis identification and follow-up, which emphasized improving the clinical nursing pathway. According to Liu and colleagues, standardization within clinical nursing pathways presents the greatest opportunity for improving SEP-1 bundle compliance and clinical outcomes.
One way to standardize nursing pathways is to systematize expectations for nursing assessments and follow-up to sepsis-related symptoms. Chmielewski and colleagues described using sepsis champions in acute care nursing departments as an option for standardization. Sepsis champions receive in-depth education on the signs and symptoms of sepsis as well as follow-up and follow through for obtaining and executing timely interventions. In addition, they serve as a resource for their respective teams. We concluded that targeting nursing for sepsis education and centralizing sepsis resources would provide the most benefit for our organization.
Deeper evaluation of the hospital’s healthcare system highlighted an evidence-based best practice consistent with recent literature—navigators to improve nursing clinical pathways. We created a new sepsis navigator position and measured (pre- and post-intervention) success in SEP-1 compliance and improvements in hospital outcomes.
What we did
In January 2022, we hired a nurse sepsis navigator into the hospital’s quality management department. We established their role and provided orientation into the quality management team.
Orientation and enculturation
Orientation to the sepsis navigator role includes completion of quality management team competencies, integration into the system, and participation in divisional sepsis and quality team meetings. This competency foundation facilitates awareness of available data reports and expectations. In addition, aligning the sepsis navigator workflow with other disease-specific navigators streamlines strategies to connect with staff, clinicians, and providers.
Standing meetings with key stakeholders (inpatient and emergency department [ED] nursing leadership and providers, frontline clinical staff) cultivates collaboration among interprofessional teams. Regular attendance at nursing councils and provider-led meetings generates awareness of the hospital’s focus on a collaborative approach to this initiative. Ultimately, these steps help the navigator understand frontline barriers to successful SEP-1 bundle implementation.
Education
The sepsis navigator must understand the data and translate it into opportunities and strengths for the clinical teams as part of the education efforts. However, education for nurses and providers differs.
The sepsis navigator targets frontline nurses at the bedside, attends staff meetings and change-of-shift huddles, and performs daily rounds to normalize conversations about the sepsis bundle components. The navigator discusses the importance of early intervention and follow-up and asks about barriers to the team’s success.
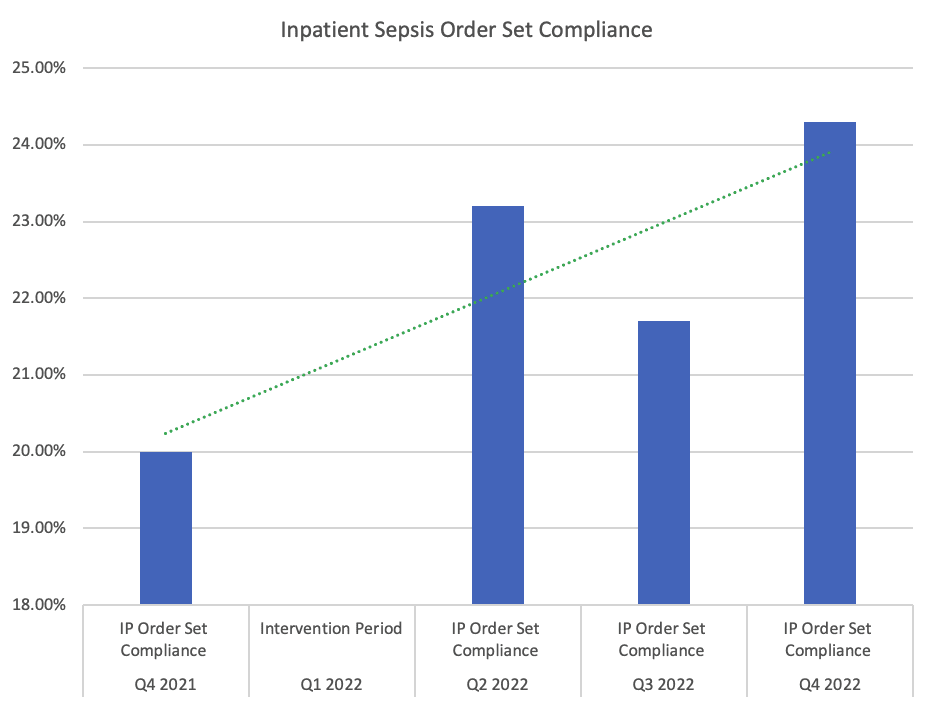
When targeting providers, the sepsis navigator partners with physician leaders, such as the ED medical director, to share the importance of using the order set and its impact on bundle compliance and sepsis mortality. Because 80% of the hospital’s sepsis diagnoses are deemed present on arrival, the navigator targeted the ED order set as a priority intervention during this pilot.
In addition to nurse and provider education, the sepsis navigator performs daily chart reviews for sepsis bundle compliance. Studying these cases and providing immediate feedback to the clinical teams allow the sepsis navigator to intervene in real-time.
Sustainment
We implemented a reward-and-recognition program to acknowledge the efforts of the care team when chart reviews reveal compliance with the SEP-1 bundle. Each month, the sepsis navigator reports SEP-1 bundle compliance and sepsis mortality data, reviews implemented interventions, and provides a plan for correction as necessary to the hospital leadership team. The hospital president, chief medical officer, and chief nursing officer review these data.
How we assessed outcomes
We measured the success of the new sepsis navigator role using the Magnet® Empirical Outcome framework for performance improvement. This method includes observing pre- and post-intervention time frames of several patient-sensitive metrics, including sepsis ED and inpatient order set use, SEP-1 bundle compliance, and sepsis mortality.
Results
This pilot facilitated several improved processes and patient outcomes. After implementing the sepsis navigator role in January 2022, the hospital’s SEP-1 bundle compliance increased 13.1% from Q4 2021 to Q4 2022. ED order set compliance improved by 11.3%, and inpatient order set compliance improved by 4.3% in the same time frame. In addition, sepsis mortality rates decreased 9%. (See Pilot outcomes.)
Limitations and future implications
The time frame of the pilot during high-census months limited the generalizability of our conclusions. Orientation for the sepsis navigator was limited due to the urgent need for an improvement in bundle compliance.
When looking at CMS SEP-1 bundle compliance, internal abstractors reviewed approximately 30% of charts for patients with sepsis; patients with COVID-19 were excluded. Inconsistent capacity surges above the hospital’s standards throughout the year presented challenges, which required the clinical team to focus on patient throughput.
Adopting a best practice
Our organization intends to adopt the sepsis navigator role as a best practice throughout the healthcare system. We’re currently reviewing the impact of the role on readmissions. The hospital may implement similar disease-specific nurse navigators to improve other patient sensitive outcomes.
All acute care hospitals should consider the implications of adopting a nurse navigator role to support improvements within sepsis-related patient outcomes with considerations for pilot repetition inclusive of COVID-19 patients spanning a larger time frame.
The authors work at Sentara Leigh Hospital in Norfolk, Virginia. Melissa A. Grootendorst is a director of patient care services. Teresa E. Bilyeu is a director of patient care services and Magnet® program director. LaVaul A. Harris is a quality improvement coordinator. Jennifer B. Kreiser is vice president and chief nursing officer.
American Nurse Journal. 2024; 19(1). Doi: 10.51256/ANJ012442
References
Centers for Disease Control and Prevention. What is sepsis? August 27, 2023 cdc.gov/sepsis/what-is-sepsis.html
Chmielewski NA, Faulkner LD, Drone M. Using floor champions to improve sepsis quality outcomes in community hospitals. Nurse Lead. 2019;17(2):151-4. doi:10.1016/j.mnl.2018.08.005
Esposito A, Silverman ME, Diaz F, Fiesseler F, Magnes G, Salo D. Sepsis core measures—Are they worth the cost? J Emerg Med. 2018;55(6):751-7. doi:10.1016/j.jemermed.2018.07.033
Gesten F, Evans L. SEP-1—Taking the measure of a measure. JAMA Network Open. 2021;4(12):e2138823. doi:10.1001/jamanetworkopen.2021.38823
Liu CX, Wang XL, Zhang K, et al. Study on clinical nursing pathway to promote the effective implementation of sepsis bundle in septic shock. Eur J Med Res. 2021;26(1):69. doi:10.1186/s40001-021-00540-8
Threatt DL. Improving sepsis bundle implementation times. J Nurs Care Qual. 2019;35(2):135-9. doi:10.1097/ncq.0000000000000430
Townsend SR, Phillips GS, Duseja R, et al. Effects of compliance with the early management bundle (SEP-1) on mortality changes among Medicare beneficiaries with sepsis: A propensity score matched cohort study. Chest. 2022;161(2):392-406. doi:10.1016/j.chest.2021.07.2167
Key words: sepsis, navigator, sepsis protocol, sepsis management