Is your practice up-to-date?
Takeaways:
- Recent studies have shown that more than 88% of nurses are using non-evidence based methods for verification of nasogastric tube placement leading to serious patient harm.
- Evidence-based best practices can be used to ensure and verify nasogastric tube placement.
ON APRIL 8, 2008, my beautiful baby boy, Grant Lars Visscher, was born.
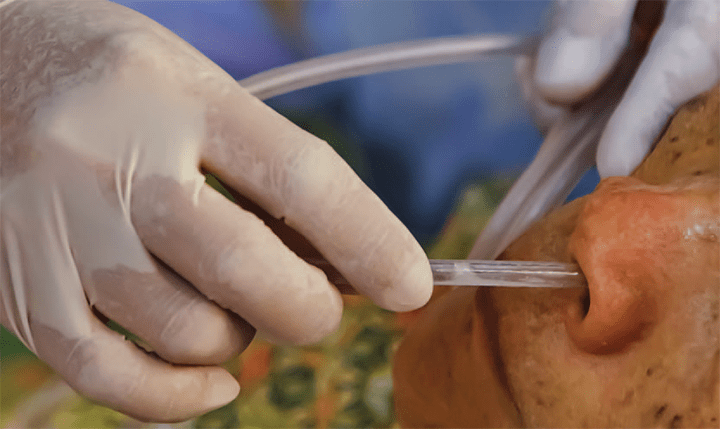
 We knew he would be born with a heart defect, so it was no surprise when he had open-heart surgery at 4 days old. As Grant was recovering, his doctors decided he would need a feeding tube to help increase his weight. With Grant just a few days old, the nurse struggled to place the feeding tube and got an X-ray to confirm placement. By the time that Grant was 11 days old, the doctors felt that he was doing so well that he would be released from the hospital in just a couple of days. But that wouldn’t happen. It was on this day that the morning nurse wasn’t comfortable with Grant’s feeding tube, and she got approval to insert a different style. As I watched her struggle to put it in, I let her know that the current tube placement was confirmed by x-ray. She told me that wasn’t needed and proceeded to insert the tube while explaining to me that she had years of experience. I asked her multiple questions about how she would know the feeding tube was placed correctly. She showed me the process of auscultation and aspiration to verify the placement.
We knew he would be born with a heart defect, so it was no surprise when he had open-heart surgery at 4 days old. As Grant was recovering, his doctors decided he would need a feeding tube to help increase his weight. With Grant just a few days old, the nurse struggled to place the feeding tube and got an X-ray to confirm placement. By the time that Grant was 11 days old, the doctors felt that he was doing so well that he would be released from the hospital in just a couple of days. But that wouldn’t happen. It was on this day that the morning nurse wasn’t comfortable with Grant’s feeding tube, and she got approval to insert a different style. As I watched her struggle to put it in, I let her know that the current tube placement was confirmed by x-ray. She told me that wasn’t needed and proceeded to insert the tube while explaining to me that she had years of experience. I asked her multiple questions about how she would know the feeding tube was placed correctly. She showed me the process of auscultation and aspiration to verify the placement.
After the tube was placed, Grant seemed off. His color changed, he blew milky white bubbles, and he seemed agitated. I mentioned it to the nurses throughout the day but none of them looked into what was causing his distress. By evening, when he was getting his feed, he was starting to turn blue around the mouth. I mentioned this to the nurse again, but she continued to push the feed before evaluating him. At this point, he had turned completely blue. She asked me to go into the hall and ask for help. I ran into the hall and said, “My son is turning blue!” And I watched as 20 staff members tried to resuscitate him. My sweet baby boy was pronounced dead at 9:10 PM.
I would later learn that the nurse had incorrectly inserted the feeding tube via Grant’s trachea. This misplaced feeding tube led to filling his lungs with fluid. If the nurse had listened to me about needing the x-ray like before or listened to my concerns, Grant would be alive. We would have celebrated Grant’s 10th birthday this year; instead, we celebrated his memory.
—Deahna Visscher
Feeding and drainage tubes, including nasogastric tubes (NGTs),are routinely used in hospitals,but they carry the risk of serious and potentially lethal complications across all patient groups;elderly patients and babies are at most risk. (See NGT facts and figures.) Despite these risks, no universal standard of practice exists for bedside verification because each verification method has limitations. This article will discuss current research, steps for improving the verification process, and best practices for NGT placement and verification. Special attention will be paid to processes in theUnited Kingdom’s National Health Service (NHS).
 A troubling report
A troubling report
The state of Pennsylvania is one of a few in the United States that mandate hospitals to report sentinel events related to NGT misplacement. A recent report published by the Pennsylvania Patient Safety Authority illustrates how prevalent misplaced NGTs are and how this issue and its complications affect patients of all ages. The study analyzed enteral feeding tube misplacements over a 6-year period and found that more than half led to complications, including death. Analysts identified 166 NGT misplacements occurring between January 2011 and December 2016. Using expanded criteria, another 16 events were found.
The study also showed the distribution of misplacements among different ages. Elderly patients between the ages of 60 and 89 years were affected the most with 68.7% of the reported misplacements. New borns and infants between ages 0 and 11 months accounted for 6.6% of reported misplacements.
Analysis of the data revealed that pneumothorax was the most common outcome of feeding tube misplacement for elderly patients. Other complications included coiling during placement, perforation, and placement in the wrong portion of the GI tract. More than half of the events (56%) were reported as serious, including two deaths. Almost half of the misplacements were discovered with a chest x-ray, which is one of the recommended practices for verification; however, of the 81 x-rays obtained, 16 were misread.
Practice improvement
Failure to detect misplaced NGTs is attributed to:
- failure to use evidence-based methods to confirm initial placement
- failure to recognize when an NGT has changed position
- failure to properly read a chest and abdominal radiograph for the “four criteria”
- Does the tube path follow the esophagus/avoid the contours of the bronchi?
- Does the tube clearly bisect the carina or the bronchi?
- Does the tube cross the diaphragm in the midline?
- Is the tip clearly visible below the left hemi-diaphragm rather than solely viewing the tip of the NGT?
- failure to accurately interpret an electromagnetic device screen.
Improving NGT placement and verification requires a two-pronged approach: consistency of radio graph ic interpretation and reporting and eliminating nonevidence-based practices.
Consistency of radiographic interpretation and reporting
Currently, x-rays are the gold standard for NGT placement confirmation because they can aid in visualizing its course. However, as Turgay noted, x-ray misinterpretation can lead to misplacement. The United Kingdom’s National Patient Safety Agency reported that between 2005and 2010, 45% of all cases of harm caused by a misplaced NGT were due to x-ray misinterpretation.
Providers without formal training in radiographic interpretation may rely solely on assessing the placement of the tube tip. Proper radiographic interpretation requires tracking the path of the tube past key anatomic points. Unfortunately, the lack of a mandated and protected central repository to report sentinel events related to NGT misplacements in the United States makes determining how often misinterpretation occurs impossible.
Eliminating nonevidence-based practices
More alarming than x-ray misinterpretation is the use of nonevidence-based practices, including aspiration or auscultation, to verify NGT placement.
Aspiration and auscultation are commonly used to verify tube placement (The American Society for Parenteral and Enteral Nutrition [ASPEN] surveyed 63 hospitals and found that 39 were using this method), but human error can result in undetected problems. Both the Child Health Patient Safety Organization and the American Association of Critical-Care Nurses (AACN) have issued alerts recommending that hospitals stop using this verification method. The basis of these alerts is that the lungs and stomach are both resonant organs that can transmit sounds, and the ability to discern the difference between them is negligible, yielding misleading results.
Research dating back to the 1990s has documented the unreliability of auscultation in verifying NGT placement. One study showed that 80% of healthcare professionals were unable to detect tubes placed in the lungs. Thirteen years ago, England banned auscultation, but in some countries, including the United States, this technique is still taught to parents, nurses, and providers.
Working toward a solution
To address concerns about lack of consistency in practice and use of unreliable verification methods,ASPEN convened a workgroup to study the issue, beginning with a focus on pediatric NGT placement verification. The New Opportunities for Verification of Enteral Tube Location (NOVEL) project is an interdisciplinary, interorganizational, andinternational effort to standardize care and to work with industry to develop technologies to addressNGT placement verification. Members of the group have critically reviewed the literature, conducted research to further describe the problem, and have developed education tools for NGT placement and verification.
Most recently, the NOVEL project has been working to create an evidence-based best practice document. The Patient Safety Movement, a nonprofit that works with global leaders in healthcare to create free resources, worked with leaders from the United Kingdom’s NHS, the NOVEL project, and Children’sHospital Colorado to create “Nasogastric feeding and drainage tube placement and verification.” This is one of the free Actionable Patient Safety Solutions (APSS) documents spearheaded by the Patient Safety Movement to address patient safety challenges (tinyurl.com/yc3d94oa).
The APSS encourages hospitals to closely scrutinize their own NGT placement and verification methods. The document includes recommendations for safe equipment, staff training and competency, institutional policies, tube placement, confirmation of placement before first use, and reconfirmation of NGT placement after initial use. The APSS also includes practices that should never be used:
- auscultation
- visual inspection of fluid from the tube
- observation of bubbles
- litmus paper.
Best practices
The APSS, based on research and best practices from the NHS and the NOVEL project, recommends evidence-based best practices to verify tube placement, including x-rays, pH testing, nose-ear-mid umbilicus measurement, and critical-thinking skills. (See Best practices.) AACN’s procedure manuals for critical care and pediatric acute care both recommend pH measurement as part of the procedure for verifying temporary NGT placement. (See Success story.)
The APSS mirrors the United Kingdom’s approach, and according to the NHS, out of about 1 million naso- and orogastric tubes inserted in England in 2017 and 2018 (based on purchase data), only 21 were misplaced in the lungs or pleura. In other words, one in 50,000 tubes was misplaced. Many experts believe that those misplacements could have been prevented using the steps outlined in the APSS.
Take action
Don’t wait for a tragic event like Grant’s to take action. If you’re a nurse leader, review the new evidence, download the recommendations, and work with others to develop and implement a plan to change current practices in your organization. If you’re not in a leadership role, share this information with the decision makers and ensure policies and procedures align with best practices. Use Grant’s story to propel this program forward and ensure that similar events don’t happen again.
Resources
|
Beth Lyman is codirector of the nutrition support team at Children’s Mercy Kansas City in Missouri. Christine Peyton is a clinical nurse specialist at Children’s Hospital Colorado in Aurora. Frances Healey is the deputy director of patient safety (Insight) at the National Health Service Improvement in London, United Kingdom.
Selected references
American Association of Critical Care Nurses(AACN). AACN practice alert: Initial and ongoing verification of feeding tube placementin adults. Crit Care Nurse. 2017;37(5):100.
Bankhead R, Boullata J, Brantley S, et al. Enteral nutrition practice recommendations. JPEN J Parenter Enteral Nutr. 2009;33(2):122-67.
Boullata JI, Carrera AL, Harvey L, et al; ASPEN Safe Practices for Enteral Nutrition Therapy Task Force, American Society for Parenteral and Enteral Nutrition. ASPEN safe practices for enteral nutrition therapy. JPEN J Parenter Enteral Nutr. 2017;41(1):15-103.
Bourgault AM, Heath J, Hooper V, Sole ML, Nesmith EG. Methods used by critical care nurses to verify feeding tube placement in clinical practice. Crit Care Nurse. 2015;35(1):e1-7.
Child Health Patient Safety Organization. Blind pediatric NG tube placements continue to cause harm. Patient Safety Action Alert. 2012.
Conway DB. Orogastric/nasogastric tube: Insertion and removal. In: Verger JT, Lebet RM,eds. AACN Procedure Manual for Pediatric Acute and Critical Care. St. Louis, MO:Saunders; 2008.
Creel AM, Winkler MK. Oral and nasal enteral tube placement and complications in a pediatric intensive care unit. Pediatr Crit Care Med. 2007;8(2):161-4.
Emergency Nurses Association. Clinical Practice Guideline: Gastric Tube Placement Verification. 2010.
Gilbertson HR, Rogers EJ, Ukoumunne OC. Determination of a practical pH cutoff level for reliable confirmation of nasogastric tube placement. JPEN J Parenter Enteral Nutr. 2011;35(4):540-4.
Healey F, Lyman B. Challenge 15: Nasogastric feeding and drainage tube placement and verification. Patient Safety Movement Foundation. July 18, 2018.
Kleinerman RA. Cancer risks following diagnostic and therapeutic radiation exposure in children. Pediatr Radiol. 2006;36(suppl 2):121-5.
Lyman B, Kemper C, Northington L, et al.Use of temporary enteral access devices in hospitalized neonatal and pediatric patients in the United States. JPEN J Parenter Enteral Nutr. 2016;40(4):574-80.
Lyman B, Yaworksi JA, Duesing L, Moore C.Verifying NG feeding tube placement in pediatric patients. Am Nurs Today. 2016;11(1).
Metheny NA, Meert KL. A review of published case reports of inadvertent pulmonary placement of nasogastric tubes in children. JPediatr Nurs. 2014;29(1):e7-12.
Metheny NA, Stewart BJ, Mills AC. Blind insertion of feeding tubes in intensive careunits: A national survey. Am J Crit Care. 2012;21(5):352-60.
National Health Service Improvement. Initial placement checks for nasogastric and orogastric tubes: Resource set. July 2016.
National Health Service Improvement. Never events data. 2018. improvement.nhs.uk/resources/never-events-data/
Ni MZ, Huddy JR, Priest OH, et al. SelectingpH cut-offs for the safe verification of nasogastric feeding tube placement: A decisionanalytical modelling approach. BMJ Open. 2017;7(11):e018128.
October TW, Hardart GE. Successful placement of post pyloric enteral tubes using electromagnetic guidance in critically ill children. Pediatr Crit Care Med. 2009;10(2):196-200.
National Patient Safety Agency. Reducing theharm caused by misplaced nasogastric feeding tubes in adults, children and infants. Patient Safety Alert. 2011.
Relias Media. Misplaced NG tubes a major patient safety risk. 2015.
Society of Pediatric Nurses (SPN) Clinical Practice Committee; SPN Research Committee, Longo MA. Best evidence: Nasogastric tube placement verification. J Pediatric Nurse 2011;26(4):373-6.
Sparks DA, Chase DM, Coughlin LM, Perry E. Pulmonary complications of 9931 narrow-bore nasoenteric tubes during blind placement: A critical review. JPEN J Parenter Enteral Nutr. 2011;35(5):625-9.
Turgay AS, Khorshid L. Effectiveness of the auscultatory and pH methods in predicting feeding tube placement. J Clin Nurs. 2010;19(11-12):1553-9.
Wallace SC. Data snapshot: Complications linked to iatrogenic enteral feeding tube misplacements. Pa Patient Saf Advis. 2017;14(4).
Wiegand, DL. Orogastric and nasogastric tube insertion, care and removal. In: AACN Procedure Manual for Critical Care. 6th ed.St. Louis, MO: Saunders; 2011.


















8 Comments.
I reviewed a CNE article in the Nov 2018 journal on reducing NG tube misplacement.
The CNE doesn’t expire until 11/1/21.
There is no button to register and submit the answers for the post test.
Thank you
I would also appreciate the PDF as my hospital cannot get an x-ray to verify placement per policy we have to call to get an x-ray ordered, I want to change that 🙂
Hi,
Please could you send me a pdf version of this article – I’d love to save it and use it as part of our research here on tube feeding in the children’s hospital.
Given the current tools and confirmation methods, nothing beats critical thinking and keen assessment of ongoing tube placement verification. The tube must maintain its location in a system which naturally moves due to peristalsis, coughing, vomiting or gagging, one can never be complacent and just believe the external “cm” measurement is unchanged so therefore the tubes in the same position.
Enteral tubes do not exist in an inert system so providers must stay awake and responsive to unexpected misplacements. External connectors help keep patients safe from external dangers but tubes need updating to alert of internal dangers or unintended movement. check out SurTube™.
This nurse has an excellent point about re-confirmation of NG tube placement. The major focus of our article is on initial placement but it is definitely important to assure the tube stays in place. She mentions tube migration and that does happen. For that reason, our nurses also document the cm mark at the naris periodically to assure the tube has not moved (at least from that point). In the ASPEN Best Practice document just published in Nutrition in Clinical Practice we do address this very issue. I agree with what she said and applaud her for commenting.
Beth Lyman RN MSN CNSC
Co-Director of the Nutrition Support Team
Children’s Mercy Hospital
As a surgical floor nurse who works with nasogastric tubes on a daily basis, it is crucial that I prevent tube displacement. Once NGT placement is confirmed, my hospital’s policy is securement of the tube and notation of the centimeter marking at the patient’s nares. The NGT is secured with a strong tape wrapped around the proximal tube and taped to the patient’s nose. The tube is also pinned to the hospital gown to prevent tugging and movement. With each encounter, the nurse should check the centimeter markings on the tube, especially during a bed-side hand-off and prior to instilling anything into the tube. Although a tube can initially be placed correctly, failure to notice accidental migration could prove to be as disastrous as a tube incorrectly placed from the start.
Amanda Desormeaux, BSN, RN-BC, CBN
A very valuable article
very good article